SAN FRANCISCO - Pancreatic imaging with CT perfusion (CTP) offers new ways to view the pancreas, unveiling dangerous tumors that are difficult to see with conventional CT and potentially offering more patients the chance for a cure, according to a talk at the International Symposium on Multidetector-Row CT (MDCT).
Among its many talents, CT perfusion can detect isodense tumors that couldn't be seen before. It can differentiate high- from low-grade tumors, distinguish adenocarcinoma from other focal lesions, and even predict response to certain therapies, said Dr. Mathias Prokop, PhD, professor and chair of radiology at Radboud University Medical Center in Nijmegen, the Netherlands, in a Wednesday session.
 Dr. Mathias Prokop, PhD, from Radboud University.
Dr. Mathias Prokop, PhD, from Radboud University.
Why perform pancreatic CT perfusion scans in the first place? "It's basically because we would like to see tumors that are very difficult to see, like isodense tumors, and for differentiation of adenocarcinoma from other tumors," Prokop said. "But also for estimating the grade of malignancy and ... selecting patients for treatment regimens, determining prognosis, and looking at follow-up to treatments." Importantly, it's easy to do, and it's available now, he added.
And while CT perfusion of pancreatic tumors was the focus of his talk at MDCT 2014, CTP is also very useful in pancreatitis, Prokop said.
"There are some publications that show you are able to see early perfusion defects that actually have a chance of becoming a pancreatic necrosis," he said.
Pancreatic tumors are tailor-made for CT perfusion because they behave like highly malignant rectal cancers in their perfusion. The vast majority of such tumors have reduced blood volume and blood flow compared to normal pancreatic parenchyma, and this feature makes CTP useful, Prokop said, citing the work of Kendel et al, who demonstrated low blood volume and perfusion in pancreatic adenocarcinomas back in 2009.
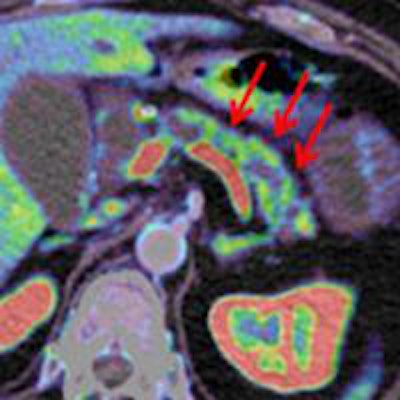
The same principle applies to the detection of tumors that are isodense to the surrounding parenchyma. These are difficult to detect even with multiphase CT, and often when they are missed "it basically means we picked the wrong phase," he said. "If you really know what you're looking for, you might be able to see something." Not so with CT perfusion, where the area shaded blue corresponds to the tumor, Prokop said.
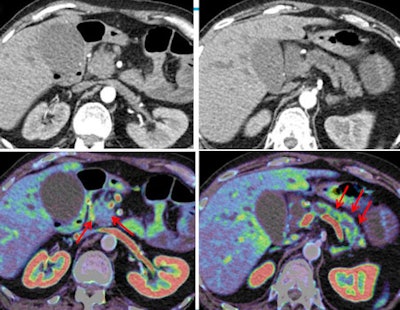 Histology-proven classic adenocarcinoma with infiltration of the duodenum seen in CTP images (bottom row) of a 67-year-old woman presenting with abdominal cramps, weight loss, and jaundice. The lesions are barely visible in conventional CT (top row). All images courtesy of Dr. Mathias Prokop.
Histology-proven classic adenocarcinoma with infiltration of the duodenum seen in CTP images (bottom row) of a 67-year-old woman presenting with abdominal cramps, weight loss, and jaundice. The lesions are barely visible in conventional CT (top row). All images courtesy of Dr. Mathias Prokop.Similarly, high-grade tumors can be distinguished by virtue of their lower blood volumes and lower peak enhancement in CTP compared to low-grade tumors, Prokop said. With CTP, "you can get sensitivity of 60% with very high specificity, which means if you have this kind of behavior, the chance of having a high-grade tumor is extremely high" -- essentially 100% positive predictive value.
Looking at enhancement curves can be helpful for differentiating adenocarcinoma from other entities. Zamboni et al showed that adenocarcinomas have quite a bit of "leakiness," meaning there's very little or no washout of contrast compared with chronic pancreatitis or neuroendocrine tumors, for example, which show some washout on enhancement curves, Prokop said.
Performing CT perfusion
The classic way to perform CT perfusion of the pancreas is to give patients oral water (1,000 mL) for contrast; this is followed by hyperventilation while the patient wears an abdominal belt to restrict perfusion and motion in the abdomen. Working in Europe where antispasmodic drugs are approved, Prokop's center traditionally adds butylscopolamine (1 mL IV) or glucagon to the patient prep to aid registration of the perfusion images, which is complicated by peristalsis. Shallow breathing is preferred during the acquisition because it's a long exam to expect a breath-hold. Motion correction performed during image preprocessing works reasonably well, Prokop said.
Patients are typically injected with 40 mL to 80 mL of contrast material prior to dynamic scanning using a low-kV technique (80 kV to 100 kV, depending on patient size):
- Arterial phase (10-40 sec postinjection): every 2-3 sec
- Portal phase (40-70 sec postinjection): every 4-6 sec
- Late phase (70-120 sec postinjection): every 10-20 sec
More scans are usually acquired during the arterial phase than the later phases, Prokop noted. Generally, a diagnostic scan performed at another time is required in addition to the CT perfusion scan.
Many paths to perfusion
Many different imaging protocols have been used in the past several years, depending on the indication and the scanner type, Prokop said.
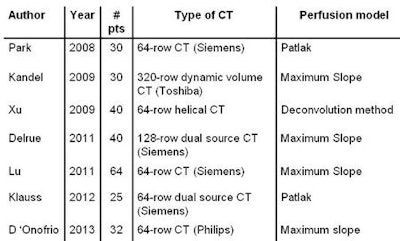 Studies over the past several years have used a wide variety of techniques for perfusion imaging.
Studies over the past several years have used a wide variety of techniques for perfusion imaging.
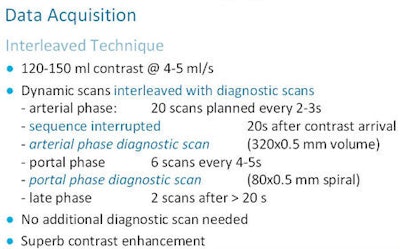 At Prokop's facility, the pancreatic CTP method of choice is the interleaved technique, which blends diagnostic with CT perfusion scans, interrupting each scan type.
At Prokop's facility, the pancreatic CTP method of choice is the interleaved technique, which blends diagnostic with CT perfusion scans, interrupting each scan type.
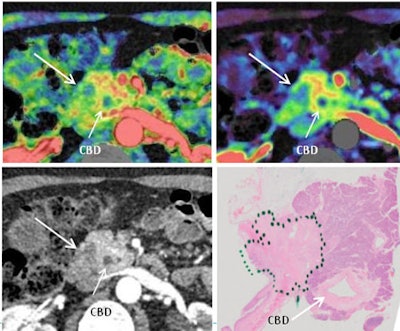 Once CTP (upper left) is registered with conventional CT images (lower left) acquired using the interleaved technique, the diagnosis becomes easy owing to the high contrast and delineation of structures, as shown for this patient with classic pancreatic cancer with common bile duct (CBD) involvement. Histology is shown at lower right.
Once CTP (upper left) is registered with conventional CT images (lower left) acquired using the interleaved technique, the diagnosis becomes easy owing to the high contrast and delineation of structures, as shown for this patient with classic pancreatic cancer with common bile duct (CBD) involvement. Histology is shown at lower right.CT perfusion is also very useful for identifying severe acute pancreatitis, Prokop said. Among 30 patients, Tsuji et al found 10 to have pancreatic ischemia, and pancreatic necrosis was found in nine of the 10. In trauma patients, CTP is also useful for detecting hypovolemic shock, characterized by low blood flow in the early phase and increased permeability (late uptake).
When it comes to techniques for performing CTP, "there's not a lot of standardization out there," he said.
Additional diagnostic scans are usually needed, but combining CTP with conventional exams in a single session offers "really superb enhancement," Prokop said. CTP distinguishes high-grade from low-grade tumors and "ultimately the response to therapy."