SAN FRANCISCO - Even the largest and most unwieldy collection of CT scanners in a multisite institution can function as one by standardizing three simple components of their CT scanning protocols, according to a Sunday presentation at the annual International Symposium on Multidetector-Row CT (MDCT).
For the Mayo Clinic in Rochester, MN, the topic wasn't hypothetical. Consolidation in the clinic's healthcare system had left the institution with no fewer than 58 different CT scanners in more than 13 centers operating with very different scanning protocols.
How do you begin to optimize dose and image quality across all of them? By standardizing in-plane resolution, axial resolution, and noise, said Cynthia McCollough, PhD, professor of medical physics and biomedical engineering at Mayo Clinic.
Getting started
The process starts with measuring and standardizing three things on every scanner, McCollough said in her opening day talk:
- Modular transfer function (MTF)
- Slice sensitivity profile (SSP)
- Image noise for a range of phantom sizes to adjust automated exposure control (AEC) settings
Using the results of these measurements to evaluate spatial resolution and image noise "can help guide you in getting image quality consistent across scanners," McCollough said.
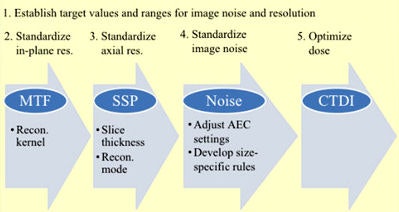 Three measurements are required to begin the process of standardizing image quality and dose across a widely divergent scanner collection. Images courtesy of Cynthia McCollough, PhD.
Three measurements are required to begin the process of standardizing image quality and dose across a widely divergent scanner collection. Images courtesy of Cynthia McCollough, PhD.Harmonizing dose and noise across a large and diverse healthcare system is a tough job considering the enormous range of patient sizes, she said. But for the sake of patient safety and clinical consistency, it had to be done.
"We wanted to determine how consistent it was or not, see what actions we could take to deliver more consistent results across this very big practice, and try to develop it in the strategic sense as something that can be repeated on an ongoing basis," McCollough said.
Beginning with measurements
The project evaluated 16 of the enterprise's 58 scanners across 10 different sites, covering three manufacturers, and measured the parameters for a routine abdomen exam. The most important thing the group did was to use three different phantom sizes, according to McCollough.
"Standardization for just the medium phantom is not standardization because we have more than medium-sized patients," she said.
 Cynthia McCollough, PhD, from the Mayo Clinic.
Cynthia McCollough, PhD, from the Mayo Clinic.They used a wire phantom to measures in-plane resolution, a foil phantom to measure z-axis resolution, and an abdominal phantom for their tests.
Next, the investigators measured spatial resolution -- both cross-plane and in the z-axis -- with the standard modulation transfer function. Then they measured image noise and recorded the console CT dose index (CTDI) readout.
A CT technologist was instructed to scan each phantom as if it were a patient, "exactly as you would do for this size patient," McCollough said. "We did it for all three phantoms, and this is important because you need to know how the scanner responds to changes in patient size."
They found kVp settings ranging from 80 to 130 kV. Scanners from Siemens Healthcare used quality-referenced mAs, while those from Toshiba America Medical Systems and GE Healthcare used standard deviation and noise index, respectively.
"We had some AECs that used size-specific technique charts and some that used just the default reference protocols that come with the scanner," she said.
Some scanners used protocols with iterative reconstruction to reduce radiation dose in their abdominal scans, while others did not. The one consistent thing was a 5-mm slice thickness, McCollough said.
As for MTF, all the scanners fell into the middle range of about a medium-sharp body kernel. "We were pleased with that because users don't have control of the kernel shape," she said.
Slice sensitivity profiles were quite different across manufacturers.
As for noise, the group decided to use the in-house data for their Siemens scanners as a reference standard, having spent time optimizing those models. The others were standardized to the Siemens models. The group looked at scanner noise behavior for small, medium, and large patients from this perspective.
As might be expected, scanning the larger patients revealed a far wider noise range among the scanners than the medium-sized patients, for all systems.
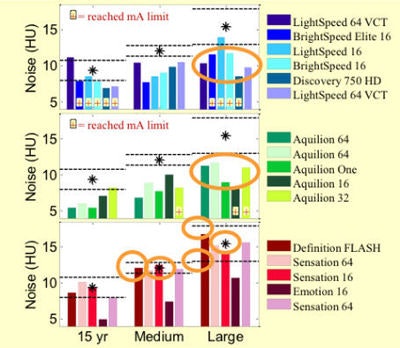 Charts top to bottom depict noise levels for GE, Toshiba, and Siemens scanners, respectively. For both Toshiba and GE, the noise values were below the chosen target, which meant that doses could be reduced.
Charts top to bottom depict noise levels for GE, Toshiba, and Siemens scanners, respectively. For both Toshiba and GE, the noise values were below the chosen target, which meant that doses could be reduced."So we've got room for optimization," McCollough said. "Since we're happy with the lower noise level, we can decrease the dose, that is, increase the noise level, on the other scanners we're working with."
Summing it up
McCollough summed up the following points from their experience:
- In-plane resolution was relatively consistent across all scanners, she said. If it had not been, the kernel would have needed to be changed.
- Image width was consistently higher for GE machines, which have a "Plus" mode that cuts noise by increasing slice width to a little over 6 mm; it should not be used when standardization is the goal.
- SSP affects image noise and should be standardized before attempting to standardize noise.
- Of all of the factors, AEC has the largest effect on image noise and is the most important parameter to standardize. Size-dependent image-noise measurements using different phantoms are essential for measuring AEC's impact.
- Image noise should increase slightly with patient size to maintain lower dose ranges.
"If you have one of those systems like GE or Toshiba that tries to maintain the same image noise across all patient sizes, [we incorporate] a technique chart and use different noise indexes and different standard deviation values as patient sizes change," McCollough said.
Iterative recon changes everything
One big fly in the ointment is iterative reconstruction.
"It changes everything because dose and noise become uncoupled in the iterative world," McCollough said.
Even though resolution may be technically unaffected, the reduced contrast seen with iterative reconstruction is worrisome because it can make low-contrast findings harder to see.
Therefore, if you use iterative reconstruction, leave it at a moderate setting, she said. If the task involves a low-contrast setting, dose should be reduced by no more than about 25%. In a high-contrast setting, dose can be reduced by about 50%.
"This is what we've done," she said.
The work is now being repeated to show a before and after picture of what has been accomplished, McCollough added.