The increased use of metallic screws and other fixation devices to repair shoulder injuries is making CT a more effective imaging option than MRI for evaluating postoperative results.
In a comparison with conventional MRI and MR arthrography, CT detected additional pathology when the presence of metallic artifacts essentially precluded an assessment of the shoulder on MRI, according to study results presented at RSNA 2015.
While these metallic screws and fixation devices are MRI-compatible, "they all cause a degree of metallic artifact," said study author Dr. Thomas Magee, a principal owner at NeuroSkeletal Imaging of Florida. "In that regard, CT has been helpful in the diagnosis of labral tears or supraspinatus tendon tears in the postoperative shoulder."
 Dr. Thomas Magee from NeuroSkeletal Imaging.
Dr. Thomas Magee from NeuroSkeletal Imaging.In general, postoperative shoulder patients are often difficult to image due to scar tissue, metallic artifacts, and anatomic abnormalities. Thus, there is some debate over how to image a postoperative shoulder accurately, Magee said.
"There are some challenges with the postoperative shoulder, in that surgeons will do some work on the shoulder and that will cause the labral, especially, to look abnormal, despite the fact that there is no tear there," he added.
When this occurs, arthrography is often an option. During an arthrogram, contrast can be injected directly into the joint for imaging by CT, MRI, or x-ray to locate a tear or to produce a more definitive diagnosis of a re-tear.
At his practice, Magee and colleagues inject x-ray dye to confirm the location of the shoulder injury and where the surgery must be performed.
"So, if there is a problem with the MRI of too much artifact, we have the option of bringing the patient to the CT scanner to make the diagnosis," he said.
Modality comparison
The study included 100 consecutive patients with a variety of injuries and abnormalities who were scanned using MRI, MR arthrography, and CT arthrography. Patients received a combination of gadolinium and CT contrast agent at the time of the arthrogram so CT could be performed after the procedure if a metallic artifact interfered with the MRI scan.
The results were reviewed retrospectively by two musculoskeletal radiologists. MRI uncovered 42 full-thickness supraspinatus tendon tears, 32 superior labral anterior to posterior (SLAP) tears, 19 anterior labral tears, and 16 posterior labral tears.
Meanwhile, MR arthrography showed 51 full-thickness supraspinatus tendon tears, 46 SLAP tears, 22 posterior labral tears, and 24 anterior labral tears. Of these, 14 SLAP tears, nine supraspinatus tendon tears, six posterior labral tears, and five anterior labral tears were not detected on conventional MRI.
Nineteen patients underwent additional imaging with CT arthrography because metallic artifacts precluded an MRI assessment of their shoulder pathology. CT arthrography found four anterior labral tears, three posterior labral tears, two SLAP tears, and one supraspinatus tendon tear.
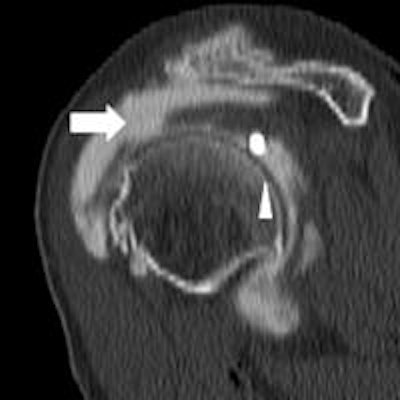
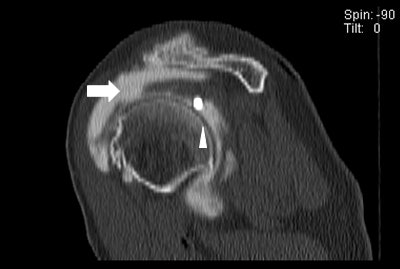 The CT image above shows a loose metallic screw (bottom arrow) and a rotator cuff tear (left arrow). The same CT below shows a second tear and loose screw (arrow). All images courtesy of Dr. Thomas Magee.
The CT image above shows a loose metallic screw (bottom arrow) and a rotator cuff tear (left arrow). The same CT below shows a second tear and loose screw (arrow). All images courtesy of Dr. Thomas Magee.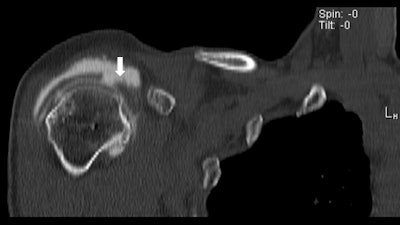
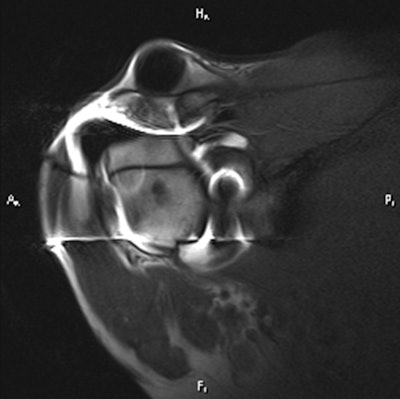 By comparison, the MR arthrogram offers virtually no details of the loose screw or rotator cuff tear.
By comparison, the MR arthrogram offers virtually no details of the loose screw or rotator cuff tear.Significant findings
Magee noted two significant outcomes of the study. The first is that MR arthrography appears to be superior to conventional MRI in detecting labral tears and supraspinatus tendon tears. The second is that CT can be essential to making the diagnosis when there is a metallic artifact.
While he is not an orthopedic surgeon, Magee said the latter conclusion is particularly significant given the rise in the use of metallic objects and implants, which can repair injured shoulders better than some older, plastic fixation devices.
"Some shoulder surgeons are starting to move toward ordering a CT arthrogram instead of an MRI," he said. "Some of the advances in CT have made the modality very good at detecting pathology in the musculoskeletal system. We have 64-detetctor-row CT that reconstructs very well with very thin [slice] imaging. It provides a good alternative to MRI."




















