A protocol using unenhanced MRI and MR arthrography can help determine which patients should receive surgery to repair labral tears, according to a study published in the November issue of the American Journal of Roentgenology.
Study author Dr. Thomas Magee, managing partner at the NeuroSkeletal Imaging Institute in Merritt Island, FL, found that all patients with displacement of at least 4 mm between the unenhanced MR images and MR arthrograms had unstable labral tears. The findings were confirmed by arthroscopy and the patients had surgical tacking.
"Stable tears are less likely to cause clinical symptoms, usually do not require surgical tacking, and often warrant no surgical intervention at all," Magee wrote (AJR, November 2015, Vol. 205:5, pp. 1056-1060).
Pitfalls of physical exams
It is challenging for surgeons to determine the stability of a labral tear based solely on a physical examination. One way to assess the injury is through arthroscopy, a minimally invasive procedure in which a surgeon inserts an arthroscope into the patient's joint.
MRI can help, but it's also difficult to evaluate the condition of a labral tear and possibly avoid an unnecessary arthroscopy using only static images. Therefore, Magee set out to evaluate whether adding MR arthrography and the criterion of a 4-mm shift in a labral tear's position would help determine stability.
"The reason for using 4 mm as a cutoff is that this degree of motion shows a definite change in labral tear position ... and is considered indicative of an unstable tear," he wrote.
Imaging protocol
The study retrospectively reviewed 150 consecutive cases in which patients received unenhanced MRI and MR arthrography between June 2013 and January 2014 to diagnose their shoulder pain. The cohort included 131 men and 19 women between the ages of 14 and 53 years (mean, 33 years). All patients had surgery within 51 days of their MRI exams, with a mean time between the scan and surgery of 21 days.
Unenhanced MRI was performed on a 3-tesla scanner (Signa, GE Healthcare) with a three-channel phased-array shoulder coil in oblique coronal, oblique sagittal, and axial planes. MR arthrography was performed on the same day immediately after the MRI exam with a mixture of approximately 15 mL of gadopentetate dimeglumine (Magnevist, Bayer HealthCare) and saline.
Two musculoskeletal radiologists retrospectively reviewed the MRI results and were blinded to arthroscopic findings at the time of their consensus review. Their interpretations were then matched with arthroscopic results. MRI scans found that 94 patients had superior labrum anterior and posterior (SLAP) tears, 53 had posterior labral tears, and 42 had anterior labral tears. All lesions detected by MRI were also evident on arthroscopy.
When unenhanced MR images were compared with MR arthrograms, 23 (28%) SLAP tears, 16 (30%) posterior labral tears, and 17 (40%) anterior labral tears had shifted 4 mm or more -- denoting instability. All patients with unstable labral tears proceeded to surgical tacking to correct the injury.
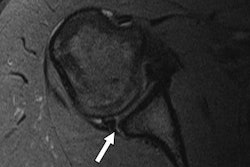
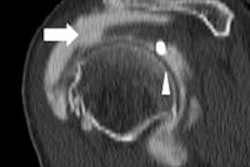
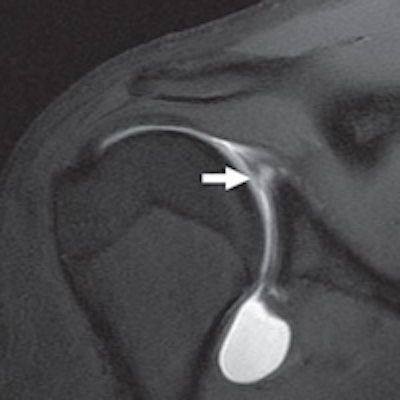
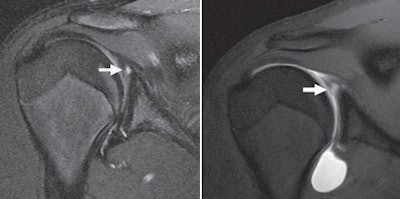 A 31-year-old man presented with shoulder pain. T2-weighted coronal MR (left) shows SLAP tear (arrow), with a T1-weighted fat-saturated coronal MR arthrogram (right) also showing a SLAP tear (arrow). There is motion of the SLAP tear by more than 4 mm, compared with unenhanced MR. Because it was ruled unstable, the tear was surgically tacked. Images courtesy of AJR.
A 31-year-old man presented with shoulder pain. T2-weighted coronal MR (left) shows SLAP tear (arrow), with a T1-weighted fat-saturated coronal MR arthrogram (right) also showing a SLAP tear (arrow). There is motion of the SLAP tear by more than 4 mm, compared with unenhanced MR. Because it was ruled unstable, the tear was surgically tacked. Images courtesy of AJR.Among the 133 labral tears that moved less than 4 mm, 130 tears (98%) were deemed stable, with confirmation via arthroscopy. The other three patients were found to have unstable labral tears at follow-up arthroscopy.
There were five SLAP tears, three anterior labral tears, and four posterior labral tears detected by arthroscopy but not seen on unenhanced MRI or MR arthrography. Those tears were considered stable at arthroscopy.
Using the 4-mm cutoff resulted in a sensitivity of 95% and specificity of 100% for detecting unstable labral tears.
| MRI and MR arthrography vs. MR arthrography alone for unstable tears | ||||
| Exam | True (false) positives | True (false) negatives | Sensitivity | Specificity |
| Unenhanced MRI and MR arthrography | 56 (0) | 130 (3) | 95% | 100% |
| MR arthrography alone | 58 (17) | 130 (1) | 98% | 88% |
There was no difference in scan time (approximately 21 minutes) between unenhanced MRI and MR arthrography versus MR arthrography alone because the same MR imaging sequences were used. The only additional time needed for unenhanced MRI and MR arthrography was due to moving the patient on and off the table.
There was a small additional cost to perform both unenhanced MRI and MR arthrography, compared with MR arthrography only. Magee estimated current Medicare reimbursement rates at $618.09 for shoulder-only MR arthrography, compared with $709.76 for both unenhanced MRI and MR arthrography of the shoulder.
In the clinical setting
At Magee's facility, technologists position a patient exactly the same way for unenhanced MRI and for MR arthrography.
"Nevertheless, there remains a possibility that the patient could be slightly differently positioned," he wrote. "This cutoff of 4 mm allows some variation in position on unenhanced MR images and MR arthrograms, therefore enabling a definitive diagnosis of motion."
Magee and colleagues routinely perform both unenhanced MRI and MR arthrography "because we believe that doing so allows better analysis of joint effusion and better analysis of labral tears," he wrote. "The unenhanced portion of the examination provides important diagnostic information for those patients who cannot complete the arthrogram portion of the examination."
Unenhanced MRI also can be useful in postoperative patients to determine the presence of a "significant metallic artifact on MRI. This can preclude MR arthrography in some cases," he added. "In those cases, we proceed to CT arthrography instead."