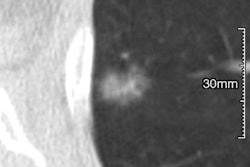
What's the best way to reduce time to treatment for patients with abnormal CT scans who are referred for suspected lung cancer? The radiology department at a Canadian hospital was able to cut the time to treatment in half for referred patients, according to a presentation at last month's Canadian Association of Radiologists (CAR) meeting in Montreal.
The radiology department at Ottawa Hospital reduced its median time to treatment from 92 days to 47 days, thanks to a complete overhaul of how lung cancer cases are managed. The facility now ranks first among 14 regional cancer centers in the province of Ontario in providing patients with a timely lung cancer diagnosis.
The staff did it by taking a number of major steps, including centralizing referral intake, educating patients about biopsies, and improving overall coordination of care, according to Dr. Carole Dennie, section head of cardiac and thoracic radiology at the hospital.
Earlier treatment
Patients with lung cancer far too often present with advanced-stage disease, which makes treatment more difficult. At Ottawa Hospital, stage IV is the most common presentation of lung cancer, with 37% of patients at that stage, Dennie noted. Median survival is only about four months for those with non-small cell lung cancer, making a 92-day time span to treatment "highly significant" for these individuals, she said.
"In the last month (of life), they are too sick to benefit from systemic therapies," she said. "Novel treatments can give patients months or even years."
Shortening the interval to treatment can create more therapeutic options for patients with advanced disease, such as making patients suitable to receive inhibitors of epidermal growth factor receptor (EGFR), said Dennie, noting that the Ottawa regional cancer program diagnoses 900 new cases of lung cancer annually.
Joint review
Before the new system was implemented, referrals were received on a variety of forms, sent to multiple destinations, and reviewed asynchronously, Dennie explained. Variable sets of procedures were ordered and scheduled independently in multiple departments. For example, a family doctor might order various tests and procedures and then refer a patient with a localized lung cancer to an oncologist rather than a thoracic surgeon. The oncologist would then have to refer the patient to a thoracic surgeon for an opinion.
"All of these independent steps introduced delays in diagnosis and treatment," she said. "Physicians also ordered multiple tests independently, and some of the tests may or may not have been necessary depending on the patient's stage at the time of initial imaging. For example, a PET/CT might be ordered on a patient who clearly had metastatic disease on the baseline CT."
With the redesigned system, a physician joint review is held the day after a referral is received that involves a thoracic surgeon, chest radiologist, and member of the clerical staff. A patient is triaged to the appropriate clinical service, be it surgical, medical, radiation oncology, or palliative care, depending on what the physicians select as a direction in treatment.
Standardized physician order sets were established to specify the type of diagnostic tests that are appropriate depending on whether the disease is localized or advanced. Advanced lung cancer (stage IV) evident on CT at the time of joint review, for example, does not warrant PET/CT, as outlined in the standardized physician order sets.
Currently, the biopsy is ordered on the day of the physician joint review, and a patient navigation day is held within two to three days after the joint review.
"As a result of the redesign, the median wait time for lung biopsies has been reduced to 10 days," Dennie said.
Patient navigation
On the patient navigation day, a nurse accompanies the patient and explains his or her patient journey, taking blood work and assessing if the patient is on any anticoagulant medications, which is addressed prior to the image-guided lung biopsy.
This is in contrast to before the revamp, when there were often patient "no shows" for those scheduled to undergo a biopsy. Clinicians attributed this to an absence of education about the role of a biopsy, Dennie said.
Patients undergo same-day imaging with modalities such as PET/CT and MRI of the brain, for those who require it, she said. The nurse also identifies any barriers to accessing care, such as the patient not having transportation to the hospital for scheduled appointments.
"Many of our patients come from a lower socioeconomic status and had difficulty getting to the hospital for their appointments," Dennie said.
Patients are also given a "patient passport" that includes all of their appointments and locations, along with a section of answers to frequently asked questions. Patients are also offered smoking cessation counseling on the patient navigation day. Almost all patients surveyed (98%) said the navigation day was helpful in setting expectations of what was to come in the ensuing weeks. The majority of patients (85%) said their tests were scheduled quickly enough.
Automated software linked to a patient's electronic medical record allows clinicians to see where a patient is in the continuum of care, Dennie noted.
"We can monitor which test [results] are coming and see if a biopsy has been scheduled or not," she explained.
A protocol for follow-up care after treatment has also been established for patients according to their stage of disease, Dennie said. As an example, patients with stage I non-small cell lung cancer who undergo surgery are scheduled to undergo a CT scan annually as follow-up care after surgery.
The interventions are being monitored to determine if the system redesign is "stage shifting" patients, Dennie said.
"We might be diagnosing patients at an earlier stage," she said. "For some patients, they might not be too ill to undergo treatment. We might be able to offer them novel therapies."
The system redesign for lung cancer referral will serve as a template for other cancer referrals at Ottawa Hospital, with the goal of shortening the time from referral to initial treatment, according to Dennie.
"We are moving this to other types of cancer at our hospital," she said. "We are now tackling hepatobiliary cancer [referrals]."