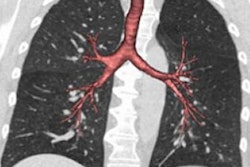
CT scans show that a quarter of the adult population has nonstandard airway branching in their lungs, which U.S. researchers have associated with an increased risk of chronic obstructive pulmonary disease (COPD). The findings were published online January 6 in the Proceedings of the National Academy of Sciences.
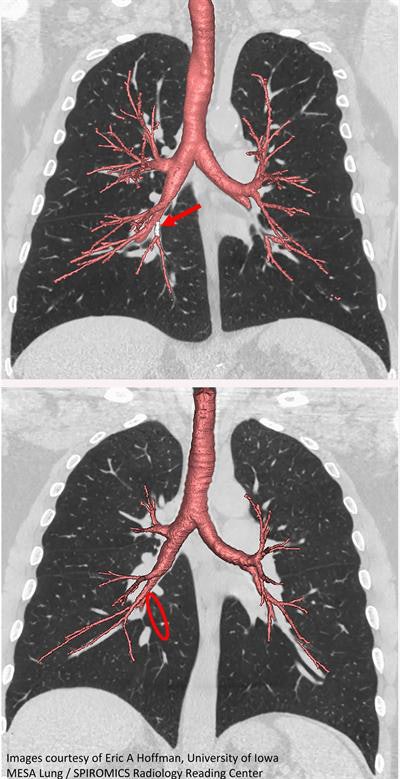 CT scan of standard central airway with medial basal airway present (red arrow; top). Absent medial basal airway variant (red circle; bottom). Image courtesy of Eric Hoffman from the University of Iowa.
CT scan of standard central airway with medial basal airway present (red arrow; top). Absent medial basal airway variant (red circle; bottom). Image courtesy of Eric Hoffman from the University of Iowa.Prolonged exposure to air pollutants such as cigarette smoke is known to accelerate a decline in lung function. The common understanding was that this deterioration was the sole cause of COPD, until recent studies showed that numerous older adults with the condition had low lung function earlier in life.
In a study funded by the U.S. National Heart, Lung, and Blood Institute (NHLBI), part of the National Institutes of Health (NIH), researchers from across the U.S. uncovered further evidence to support the idea of early proclivity to COPD. After examining more than 5,000 CT scans of patients, they found that 26.5% of the population had lung airways following nontextbook patterns that did not change throughout a 10-year period.
One of these variants in airway branching was associated with COPD among smokers and nonsmokers, the researchers found. They also identified an airway branch variation among only smokers that linked them to COPD and arose within families. The team plans to explore the genetic basis for this particular familial variation -- one of the primary targets being the FGF10 gene.
Further research is required to determine the extent to which preventive or therapeutic interventions based exclusively on innate airway branch differences could improve patient outcome, according to the group.