Radiologists should consider multiple issues when analyzing medical images used as part of gender affirmation surgeries, according to a primer on the topic issued online ahead of print on August 15 by the American Journal of Roentgenology.
The primer is being published amid rising awareness of gender dysphoria (also known as gender incongruence), in which the gender people identify with is not the one they were born with. The authors noted that gender incongruence is now categorized as a sexual health condition -- no longer as a mental illness -- in the most recent revision to the International Classification of Diseases.
Gender affirmation surgery involves the surgical alteration of an individual's physical appearance and function to resemble the identified gender, and there are three major surgical categories of gender affirmation surgery: genital reconstruction, body contouring, and maxillofacial contouring. All medical subspecialties should be prepared to identify radiology correlates and distinguish key postoperative variations in these types of surgeries, according to the authors, led by Dr. Florence Doo of Mount Sinai West in New York City (AJR, August 15, 2019).
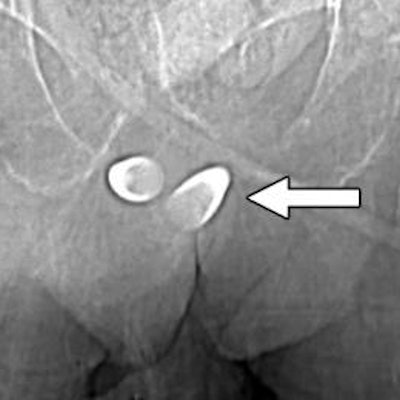
 Scout image from contrast-enhanced CT scan shows erectile implant. Stainless steel and silicone anchors (arrow) transfixed to pubic bone are asymmetric. Image courtesy of AJR.
Scout image from contrast-enhanced CT scan shows erectile implant. Stainless steel and silicone anchors (arrow) transfixed to pubic bone are asymmetric. Image courtesy of AJR.For transgender women, a form of genital reconstruction called vaginoplasty is common. The two most frequent complications of the procedure are hematomas and fluid collection; MRI is the most reliable modality to evaluate these conditions. Cellulitis, abscess, neovaginal prolapse, and focal skin necrosis can also occur. With respect to body contouring, transgender women can receive silicone or saline breast implants that often appear as incidental notations on chest x-ray, CT, and MRI scans.
The most common body contouring surgery is subcutaneous mastectomy, in which the nipple-areola complex is preserved. This preservation retains the risk of malignant transformation, so Doo and colleagues advised that transgender men undergo postsurgical breast cancer screening. Transgender women who have received neoadjuvant hormone replacement therapy should also be routinely screened due to an increased cancer risk.
Maxillofacial contouring is also used in gender affirmation surgery, and preoperative medical imaging can be used to assess the anatomical need for frontal eminence reduction. Surgeons frequently reference skull radiographs to evaluate sinus cavity size and anterior table thickness, according to the authors.
In addition, silicone injections can show up on imaging exams, as well as facial augmentations achieved via neurotoxin injections or fillers, such as calcium hydroxylapatite or hyaluronic acid.
Doo and colleagues explained that unless complications occur, postoperative images are often not acquired after gender affirmation surgery, as aesthetic results can be evaluated by surgeons. As a result, "radiologists may typically see incidental uncomplicated postsurgical findings on routine head and neck imaging," they wrote.




















