More than 70% of patients who contract COVID-19 show thickened lung tissue on chest CT exams performed six months later, a group of researchers from Italy reported in an article published online July 27 in Radiology.
 Dr. Damiano Caruso, PhD.
Dr. Damiano Caruso, PhD.And combining clinical data with baseline chest CT exam findings is an effective way to predict which COVID-19 patients are at higher risk of these types of long-term effects, wrote a team led by Dr. Damiano Caruso, PhD, of Sapienza University of Rome.
"[Our study found that] at six-month follow-up, 72% of patients showed late sequelae, in particular fibrotic-like changes," the team wrote. "Baseline LSS [Lung Severity Score] and QCCT [quantitative chest CT] of well-aerated lung showed an excellent performance in predicting [these] changes at six-month chest CT."
Chest CT findings for COVID-19 have been thoroughly explored, but mostly as they manifest in the short- and midterm of disease progression, the team noted. Further research on the disease's long-term effects is needed.
Caruso's group sought to add to the knowledge base regarding COVID-19's lasting sequelae and to investigate whether baseline chest CT findings and/or clinical data could help predict whether patients will have lung thickening at six-month follow-up.
The team conducted a study that included 118 patients who had moderate to severe COVID-19 disease between March and May 2020 (all patients' disease was confirmed by reverse transcription polymerase chain reaction [RT-PCR] testing). All underwent baseline chest CT exams and follow-up exams at six-months; the researchers assessed the exams' qualitative findings, LSS, and QCCT measures, comparing them with baseline CT exam findings. The team assessed three strategies for predicting long-term COVID-19 effects: clinical data alone, radiological data alone, and a combination of the two methods.
At six-month chest CT follow-up, 72% of patients had fibrotic-like changes in their lungs and 42% showed ground-glass opacities. The investigators found that baseline LSS and QCCT scores were effective predictors of fibrotic-like changes at this follow-up exam.
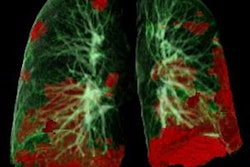
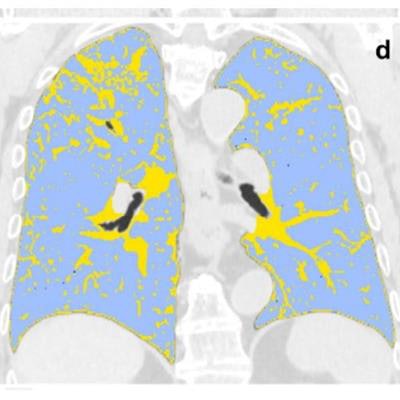
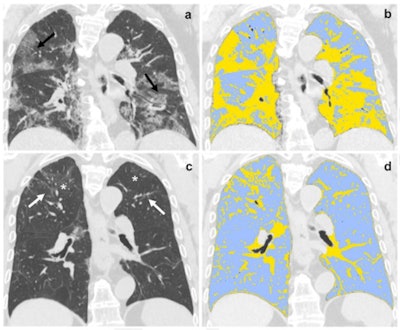 (a,b) Baseline and (c,d) six-month follow-up coronal thin-section unenhanced chest CT scans of 79-year-old man, admitted to the emergency department presenting fever, dyspnea, and cough; COVID-19 was confirmed by RT-PCR testing. (a) Chest CT scan shows bilateral ground-glass opacities tending to consolidation (black arrow). (b) The same scan after QCCT analysis highlighted in light-blue well-aerated lung (1.5 liters, 50%) and in yellow pulmonary injury of COVID-19 pneumonia. (c) Six-month follow-up scan shows residual fibrotic-like changes (white arrows) and persisting of low-density ground glass (asterisks). (d) The same scan after QCCT analysis highlighted in light-blue well-aerated lung (3.5 liters, 82%) and in yellow residual findings of COVID-19 pneumonia at six months follow-up. Images and caption courtesy of the RSNA.
(a,b) Baseline and (c,d) six-month follow-up coronal thin-section unenhanced chest CT scans of 79-year-old man, admitted to the emergency department presenting fever, dyspnea, and cough; COVID-19 was confirmed by RT-PCR testing. (a) Chest CT scan shows bilateral ground-glass opacities tending to consolidation (black arrow). (b) The same scan after QCCT analysis highlighted in light-blue well-aerated lung (1.5 liters, 50%) and in yellow pulmonary injury of COVID-19 pneumonia. (c) Six-month follow-up scan shows residual fibrotic-like changes (white arrows) and persisting of low-density ground glass (asterisks). (d) The same scan after QCCT analysis highlighted in light-blue well-aerated lung (3.5 liters, 82%) and in yellow residual findings of COVID-19 pneumonia at six months follow-up. Images and caption courtesy of the RSNA.
| Performance of three different strategies for predicting fibrotic changes in COVID-19 patients at six-month follow-up | |||
| Measure | Clinical data | Radiological data | Combination |
| Area under the curve | 0.89 | 0.81 | 0.92 |
| Sensitivity | 82% | 84% | 100% |
| Specificity | 93% | 67% | 73% |
However, in an accompanying editorial, Dr. Athol Wells and colleague Dr. Anand Devaraj, both of Imperial College London in the U.K., suggested that Caruso and colleagues may not be approaching assessment of post-COVID-19 lung changes in the most effective way.
"Each and every participant with residual disease at six months had a positive 'fibrotic-like' score: Quite simply, the prediction of 'fibrotic-like' abnormalities from baseline data was no more than a prediction of the presence of residual disease," they wrote. "The apparent increase in the prevalence of [these changes] at six months is highly deceptive, as baseline scans were performed at admission, not when the disease was most severe. ... A more progressive lung fibrosis hypothesis post-COVID would instead require evaluating change from baseline CT performed at discharge from intensive care or hospital discharge."