Poor oversight of resident physicians may have contributed to the death of a patient with lung cancer at a U.S. Department of Veterans Affairs (VA) hospital in New Mexico. A VA report on the case said the patient waited twice as long for a follow-up CT scan as should have been the case.
The report was released by the VA's Office of Inspector General (OIG) after an investigation into the death of a patient who died at the Raymond G. Murphy VA Medical Center in Albuquerque. In addition to criticizing resident follow-up, VA investigators also found fault with the quality of teleradiology connections between the hospital and teleradiologists working under contract.
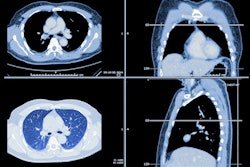
The patient had a history of smoking and was being seen for surveillance of cancer in the summer of 2017 at the hospital; a CT scan of the abdomen and pelvis had been ordered. The radiologist noted a possible spiculated nodule and recommended a follow-up chest CT scan in 90 days.
The order was relayed to the resident who had ordered the original scan, but the recommendation was not acted on until late 2017, when another resident noted the results. There was no documented evidence of oversight of the decision to order a CT scan, nor any follow-up on the CT findings by a supervising provider, according to the OIG report.
It ultimately took 175 days for a chest CT scan to be completed; the scan noted resolution of the spiculated lung nodule, but it also showed lung opacities that could indicate a possible cavitary infection or lung cancer. A PET/CT scan was ordered, but another six weeks elapsed before this scan was completed.
The PET/CT scan indicated a lesion in the apex of the right lung that appeared to be invading the chest wall and extending into the spinal canal; it appeared to be putting pressure on the spinal cord. The radiology report noted that the lesion was apparently a primary malignancy.
The patient was scheduled to be seen in the hospital's pulmonary clinic in the spring of 2018 but soon presented to the emergency department (ED) with worsening symptoms. ED physicians did not review the patient's imaging results, and the patient was sent home. After symptoms continued to worsen, a physician fellow from the pulmonary department called the patient and discussed the symptoms; a biopsy was not ordered. Instead, the fellow prescribed an infection workup and antibiotics.
The patient continued to decline and eventually sought care at two non-VA hospitals. A biopsy was performed, and a cancer diagnosis was rendered six weeks after the PET/CT scan had been interpreted.
VA investigators said that while deficiencies in the follow-up of imaging results and clinical decision-making delayed the patient's diagnosis, it was not clear if the patient's outcome would have changed with a faster diagnosis. Given the patient's age and smoking history, the discovery of a lesion in the lung warranted "prompt and thorough evaluation." A literature review indicated that lung cancer cases typically had a median time of 52 days from presentation to treatment -- that time was 110 days in this case.
The VA report faulted inadequate oversight by a supervising healthcare provider as the reason for the delay, which was compounded by the failure of residents to follow up in a timely manner on abnormal scan results. The report included a number of recommendations to the director of the Albuquerque VA hospital for better supervision of care provided by residents and fellows, as well as between departments like primary, emergency, and specialty care.
The OIG also found fault with teleradiology connections at the facility, noting that teleradiologists working under contract did not have the same level of access to prior relevant images as radiologists working at the facility.