Healthcare insurance firms may be paying too much for imaging services -- with maximum negotiated prices for some exams almost four times as high as minimum ones, a study published October 18 in Radiology suggests.
The study results may mean that insurers are passing these inflated costs along to patients, said study co-author Ge Bai, PhD, of Johns Hopkins Carey Business School in Baltimore in a statement released by the RSNA.
"High prices paid by commercial plans eventually come back to bite U.S. employers and workers through high premiums and out-of-pocket costs," she said.
Hospitals tend to have agreements with multiple insurers. And although the U.S. Centers for Medicare and Medicaid Services' (CMS) 2021 Hospital Price Transparency Rule requires hospitals to reveal pricing information, variations on prices for imaging services continue, noted a team led by John Jiang, PhD, of Michigan State University in East Lansing.
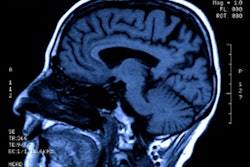
Jiang and colleagues sought to evaluate this variability among private payers for 13 radiology services using June 2022 information taken from Turquoise Health, a data platform firm.
They found that insurance firms often negotiated different prices for the same services in the same hospital. On average, the maximum negotiated price for "shoppable" radiology services was 3.8 times the minimum negotiated price in the same hospital and 1.2 times in the same hospital-insurance-company duo.
Advanced imaging exams such as CT and MRI had wider variations and higher prices compared with Medicare fees and to other imaging studies. For example, 25% of hospital-insurer pairs showed a maximum negotiated price more than 2.4 times their minimum negotiated price for brain CT.
It's clear that resolving the issue of price discrepancies in imaging will be tricky, as it could involve revamping the current hospital payment framework, wrote Dr. Ronald Arenson of the University of California, San Francisco, in an accompanying editorial.
"Imaging, especially in the outpatient setting, has been a great source for revenue and profit for hospitals in the past," he noted. "With competition from price sensitivity and increasing out-of-pocket expenses for patients, the ability for hospitals to profit from imaging has been reduced. Therefore, what was viewed as a profit center for the hospital is now viewed more and more as a cost center with little expectation for generating profits."