Obesity appears to improve the overall postsurgery survival of patients with non-small cell lung cancer (NSCLC) by 21% compared with their nonobese peers, according to study results published January 28 in Radiology.
The findings point to an "obesity paradox" -- that is, the fact that obesity may actually protect patients from poorer outcomes in certain diseases, wrote a team led by Ji Hyun Lee, MD, PhD, of Sungkyunkwan University School of Medicine in Seoul, Korea.
"[The] obesity paradox … is particularly notable in a cohort of patients with lung cancer who have undergone surgery," the group explained. "Despite ongoing debate and methodologic concerns, such as confounding factors and reverse causation, the mechanism underlying this paradox in cancer remains largely unexplored and poorly understood."
Understanding the association between improved lung cancer outcomes and obesity in patients with NSCLC requires a thorough evaluation of skeletal muscle health, but few studies have been conducted on this topic. To address this knowledge gap, Lee and colleagues investigated any associations between body mass index (BMI)-defined obesity and survival in patients with NSCLC who underwent surgery for the disease, focusing specifically on the status of skeletal muscle assessed on CT imaging.
Their research included 7,076 NSCLC patients who had surgery for it between January 2008 and December 2019. Patients were categorized into two groups: nonobese (BMI of less than 25, n = 4,564, or 64.5%) or obese (BMI equal to or greater than 25, n = 2,512, or 35.5%); clinicians assessed their skeletal muscle status via CT imaging of the third lumbar vertebrae.
Out of the total patient cohort, 22% died from NSCLC, but the obese group had a 21% decreased risk of death compared with the nonobese group.
The investigators also reported the following:
- Obese patients without low skeletal muscle mass or myosteatosis had longer overall survival compared with those in the nonobese group (HR, 0.77, p = 0.001).
- The overall survival benefit of obesity manifested in particular patient groups, namely male patients (hazard ratio, [HR, with 1 as reference] 0.72, p < 0.001); those who had ever smoked (HR, 0.71, p < 0.001); and those who did not have low skeletal muscle mass and myosteatosis. (This effect varied according to sex and smoking status, with a range of p < 0.001 to 0.02.)
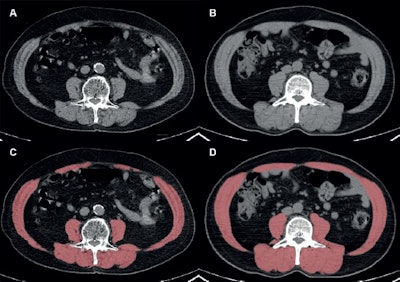 Automated segmentation of skeletal muscles at the level of the third lumbar vertebra in two representative patients with similar body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) and different skeletal muscle statuses. (A, C) Axial noncontrast CT image (A) and red overlay image (C) at PET/CT in a 68-year-old male patient with a BMI of 28.1 show low skeletal muscle mass and myosteatosis, characterized by a skeletal muscle index of 44.2 cm2/m2 and a skeletal muscle radiodensity of 26.8 Houndsfield units (HU). (B, D) Axial noncontrast CT image (B) and red overlay image (D) at PET/CT in a 69-year-old male patient with a BMI of 28.4 show normal skeletal muscle mass and radiodensity, as indicated by a skeletal muscle index of 62.4 cm2M/sup>/m2 and a skeletal muscle radiodensity of 41.6 HU. Images and caption courtesy of the RSNA.
Automated segmentation of skeletal muscles at the level of the third lumbar vertebra in two representative patients with similar body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) and different skeletal muscle statuses. (A, C) Axial noncontrast CT image (A) and red overlay image (C) at PET/CT in a 68-year-old male patient with a BMI of 28.1 show low skeletal muscle mass and myosteatosis, characterized by a skeletal muscle index of 44.2 cm2/m2 and a skeletal muscle radiodensity of 26.8 Houndsfield units (HU). (B, D) Axial noncontrast CT image (B) and red overlay image (D) at PET/CT in a 69-year-old male patient with a BMI of 28.4 show normal skeletal muscle mass and radiodensity, as indicated by a skeletal muscle index of 62.4 cm2M/sup>/m2 and a skeletal muscle radiodensity of 41.6 HU. Images and caption courtesy of the RSNA.
Why might obesity improve post-surgical outcomes in NSCLC patients? Perhaps because "metabolically healthy individuals tend to exhibit a higher proportion of skeletal muscles with normal radiodensity," the researchers wrote, noting that "improved survival in this group could be attributed to the protective effect of metabolic health against the adverse impact of obesity."
In any case, the association between obesity and lung cancer remains complex, noted Michael W. Vannier, MD, professor emeritus of radiology at the University of Chicago, in an accompanying commentary.
"[This] study … shows that the use of BMI to measure adiposity is limited and should be augmented with sarcopenia metrics," he wrote.
The complete study can be found here.