Reducing radiation dose during interventional procedures is vital for both the patient and the practitioners. Radiation-induced skin injury is one of the potential complications possible with fluoroscopically guided interventional procedures. Reducing the skin dose requires the clinician to utilize techniques and tools to minimize both the total dose and the peak skin dose.
In a review published by Radiology Online (September 13, 2002), authors Drs. Donald Miller, Patrick Noonan, Jeffrey Georgia, and Stephen Balter, Ph.D., from the National Naval Medical Center and National Cancer Institute in Bethesda, MD, and Lenox Hill Hospital in New York City describe how they minimized skin dose during interventional radiology procedures.
"Minimization of peak skin dose requires the use of both standard methods to reduce total dose and specific methods to reduce peak skin dose. Both are important, and neither alone is sufficient. Both require active operator awareness and participation," wrote the authors.
Tools
Fluoroscopy time is the only method required by the U.S. Food and Drug Administration for the estimation of patient radiation dose. U.S. fluoroscopic equipment manufacturers supplement timer functions with acquisition frame counters that indicate the number of obtained images. According to Miller and colleagues, these tools suffer from a number of drawbacks in accurately calculating patient dose.
"They provide no information regarding x-ray field size or position. They do not account for differences in dose rates resulting from differences in equipment, technique, or patient size. In general, time measurements do not provide the means for an accurate estimate of dose," they said.
In the European Union, dose-area product (DAP) measurement capabilities are required on all fluoroscopic equipment sold there. The technology is also available on interventional equipment sold in the U.S., usually as an option. DAP, which measures units of grays x square centimeters to express the total x-ray flux in the beam, is a good measure of total radiation dose, if the patient intercepts the entire irradiated field.
However, as a tool to measure peak skin dose, the tool comes up short, said the authors.
"A large dose delivered to a small skin area yields the same DAP as a small dose delivered to a large skin area. Estimation of absorbed skin dose from DAP data has a potential error of at least 30%-40%," they noted.
The interventional reference point (IRP) as a means of calculating the cumulative dose delivered at a defined point in space has been introduced by the International Electrotechnical Commission. According to the researchers, although the IRP is valuable, there are many factors mitigating its use as a tool for estimating skin dose.
"Depending on the patient’s size, the table height, and the angulation of the beam, the IRP may be outside the patient, may coincide with the skin surface, or may be inside the patient. The IRP moves relative to the patient as beam position changes. Because of these factors, cumulative dose is usually an overestimate of peak skin dose," they observed.
Real-time skin-dose measurement tools, such as radiolucent probes or scintillation dosimeters, are possible only at one or a few selected points on the skin. Because of the complexity in determining skin-dose distribution, picking the specific spot to place the measurement unit can rarely be predicted, noted the researchers.
Tools such as thermoluminescent dosimeter arrays or low-sensitivity film can be employed to measure peak skin dose, but results are not available until after the procedure has been completed. Although useful for retrospective analysis, they provide no feedback to the interventionalist during the critical procedure operation time.
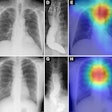
Miller and his team recommend the use of a software-based method for real-time calculation and display of a skin-dose map and peak skin dose. The product, CareGraph (Siemens Medical Solutions, Malvern, PA) is currently available as an option on some interventional systems, they said.
"Unlike other techniques, the use of dose-mapping software produces consistent results and does not require any special equipment. Its disadvantage is that the patient’s skin is mathematically modeled to a standard body phantom of the same height and weight. This model may not represent the patient’s anatomic contours exactly," said Miller and Balter in a related article in the Journal of Vascular and Interventional Radiology (April 2002, Vol. 13:4, pp. 391-397).
Technique
No matter how good the tool used to measure skin dose, dose reduction requires the interventionalist to adhere to basic fluoroscopic dose practices. These include controlling the fluoroscopy time, controlling the number of obtained images, and controlling the technical factors. All of these are the direct responsibility of the interventionalist.
Technical factors that can be optimized on any fluoroscopic device include maximizing source-to-skin distance, minimizing the air gap between the patient and the image intensifier, and limiting the use of electronic magnification, said the authors. They advocate the assistance of a medical physicist to ensure that beam filtration, grid removal (when appropriate), and adjustment of fluoroscopic voltage (kVp), and fluoroscopic and digital imaging dose settings are also optimized on the device.
The researchers strongly support the use of dose-saving pulsed fluoroscopy whenever possible. In their work, at a rate of 15 or 7.5 pulses per second, they were able to decrease the fluoroscopic dose rate by 47% and 72% respectively, compared with the dose rate at conventional fluoroscopy.
In addition to reducing total radiation dose to the patient, as well as the interventionalist and assistants, there are two techniques that Miller and his team used to reduce peak skin dose.
"The first technique is to change the position of the radiation field on the patient’s skin by using gantry angulation, table movement, or both. The second technique is to reduce the size of the radiation field by using collimation. The purpose of these techniques is to spread or "smear" the skin dose over as large an area as possible. Spreading the administered dose over a larger area accomplishes two things. First, it reduces peak skin dose. Second, it reduces the area of skin subjected to the peak skin dose," they wrote.
They group noted that even if it is not possible to reduce peak skin dose below 2 Gy (the threshold dose for the erythema), dose spreading may decrease the size of the skin area that receives the peak skin dose.
Collimation is equally as important as dose spreading because different irradiated fields can overlap on the skin surface. If optimal collimation is employed during the procedure, overlap may be prevented, and the effectiveness of dose-spreading techniques is improved, said the researchers.
There is no doubt that every prudent interventional radiologist strives to minimize the radiation dose for every procedure. However, no matter how careful and prudent they are with their planning, tools, and technique, there are some instances in which dose rates will be higher than desired.
"Patient factors, anatomic variations, disease complexity, and the type of procedure may combine so that a prolonged procedure with a high radiation dose is unavoidable. This is not necessarily a contraindication to performing or continuing a procedure. It also does not necessarily indicate poor technique on the part of the operator. As with all of medicine, it is necessary to consider all of the benefits and risks of the fluoroscopically guided procedure, as well as all of the benefits and risks of alternative therapies, if any are available," noted the researchers.
By Jonathan S. BatchelorAuntMinnie.com staff writer
October 11, 2002
Related Reading
Protective device makes interventional procedures safer for radiologists, September 13, 2002
Three simple steps can reduce interventional x-ray dose, April 9, 2002
New protective devices shield interventional radiologists, February 5, 2002
CT dose study is good news for interventional radiologists, October 5, 2001
Low-dose CT fluoroscopy minimizes interventional exposure, July 30, 2001
Copyright © 2002 AuntMinnie.com