While establishing the feasibility of digital radiography (DR) for lung cancer screening, a Dutch study has questioned the practicality of DR as a substitute for CT in detecting lung masses, according to a study published in the May issue of Radiology.
The research underscores the relative diagnostic inefficiency of DR compared to CT, and the importance of physician experience and training for optimizing DR's efficacy, according to first author Dr. Bartjan de Hoop, a radiology resident at University Medical Center in Utrecht, the Netherlands (Radiology, May 2010, Vol. 255:2, pp. 629-637).
"We show it is more efficient to do a low-dose CT than it is to do a digital radiograph," he said in a phone interview.
Though several highly publicized trials have established the ability of CT to detect early-stage lung cancers, DR remains under consideration as a screening tool because it costs less and exposes patients to far less ionizing radiation than CT. Older studies of radiography-based chest screening produced poor results, but that research used analog x-ray -- modern DR with postprocessing tools might make radiography more suitable for screening.
However, de Hoop's study indicates that radiologists still have to rely heavily on CT to generate enough reader confidence to trust DR for initial lung cancer diagnosis.
NELSON patients
The study was developed by Dr. Cornelia Schaefer-Prokop, Ph.D., at Utrecht University and Dr. Mathias Prokop, Ph.D., at the Meander Medical Center in Amersfoort, the Netherlands. Their collaborations with radiologists and pulmonologists at University Medical Center Utrecht, University Medical Center Groningen, the Academic Medical Center in Amsterdam, and Erasmus Medical Center Rotterdam -- all in the Netherlands -- and University Hospital Gasthuisberg Leuven in Belgium have led to numerous studies published recently on the relative value of DR and CT for pulmonary applications.
This work includes the Dutch-Belgian Randomized Lung Cancer Screening Trial (NELSON), a longitudinal, multicenter study evaluating the effect of annual CT lung screening on lung cancer mortality. The decade-long evaluation involves 7,557 smokers who receive annual screenings and another 7,000 high-risk subjects who serve as controls.
The NELSON trial has entered its fourth year of testing. Preliminary results have determined that the sensitivity of CT is 94.6%, and its negative predictive value for ruling out malignant disease among suspicious nodules is 99.9% (New England Journal of Medicine, 2009, Vol. 361:23, pp. 2221-2229).
For the DR study, 55 patients with histologically confirmed lung cancer and 72 control subjects deemed cancer-free were recruited retrospectively from 4,938 patients who underwent baseline and one-year follow-up screening for the NELSON trial. All had received DR lung cancer exams within two months of CT screening.
Four radiologists with varying levels of experience evaluated posteroanterior and lateral views acquired with DR and assessed their findings on a five-point confidence scale. Level 1 meant the reader was highly confident that no lesion was present. Level 5 meant the reader was highly confident that a lesion was definitely present. Efficacy rates for each reader at each confidence level were calculated.
Twenty-four (44%) malignancies were correctly localized by the four physicians. At level 5, for example, the sensitivity of DR for correctly localized malignant lesions ranged from 18% to 49% at a specificity of 100%. The false-positive rates in the control group ranged from 0% to 13%.
Seven (13%) metastatic lesions were missed by all observers, and three of the seven remained undetectable on the radiographs even when CT findings were known. Depending on reader experience, de Hoop and colleagues concluded that 22% to 63% of the lung cancers detected with CT would have been missed if chest DR had been used alone.
Still, the researchers found that DR can equal the 94% lung cancer detection rate achieved with CT screening, but this high level of performance requires an experienced or well-trained reader and must be delivered at the expense of a high false-positive rate.
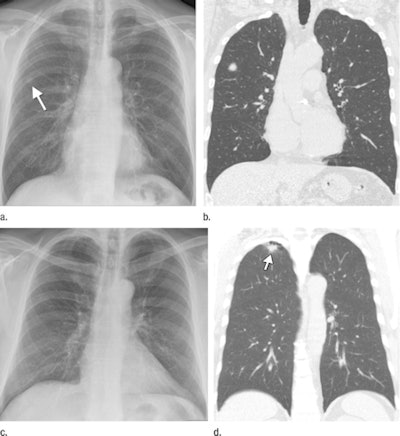 |
| (a) Digital radiography can localize lung cancers, such as an 11.4-mm diameter malignancy considered as definitely present in separate readings by three radiologists and a radiology resident. (b) Tumor's presence is confirmed with CT. (c, d) But lung malignancies can be undetectable with DR, even when their presence on CT had been previously disclosed to the observers. Images provided by Dr. Bartjan de Hoop; republished with permission of the Radiological Society of North America. |
In the trial, the reader who achieved the highest diagnostic yield with DR was a chest radiologist with more than 20 years of clinical experience. A general radiologist, who also practiced for more than 20 years, did not perform as well as a third-year radiology resident who was specially trained to read the scans.
To achieve a 94% detection rate, 62 follow-up CT exams were required for all patients, except those with level 1 DR scans showing no irregularities. Had this standard been applied to subjects in the NELSON trial, 3,191 CT exams would have been required, and three cancer cases still would have have escaped detection, the authors reported.
"This finding shows that even modern digital chest radiography has a much worse performance than does CT for lung cancer screening and is hampered by large numbers of false-positive readings or low detection rates," the authors wrote.
By James Brice
AuntMinnie.com contributing writer
April 27, 2010
Related Reading
Will new DR technologies offer alternative to CT? Part 2, March 25, 2010
Will new DR technologies offer alternative to CT? Part 1, March 24, 2010
Low-dose tomo beats chest DR for TB evaluations, March 19, 2010
Virtual dual-energy DR improves lung lesion detection, February 10, 2010
Rads prefer dual-energy x-ray over standard DR in lung, January 29, 2009
Copyright © 2010 AuntMinnie.com