Computed radiography (CR) with temporal subtraction has proved more accurate than CR alone or chest CR with double reading in a study from Japan. The observer performance trial used exams from a 12-year archive of mobile lung cancer screenings.
While lung screening with imaging is still controversial in the U.S., the Japanese have long shown confidence in advanced imaging technologies for this application, as well as for tuberculosis and other potentially lethal diseases.
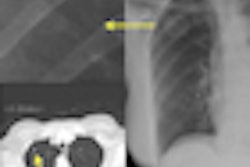
Temporal subtraction is a digital x-ray technique in which two digital images are acquired at different times; by using digital image processing, clinicians can subtract one image from another. The technique can be useful for following interval changes through the elimination of normal structures such as ribs and pulmonary vessels, according to the authors.
But despite temporal subtraction's potential utility, the authors said they did not know of any previous research that examined the use of the technique in a clinical setting for lung cancer screening.
To that end, the group conducted a study that assessed the technology in lung cancer screenings performed from 1997 to 2008 in the largely rural Iwate Prefecture in the northeast region on the main island of Japan. Some 186,340 lung cancer screenings were performed from a mobile van equipped with a CR reader with temporal subtraction capabilities (FCR 9501, Fujifilm Medical Systems). Results were published in the January 2011 issue of Radiological Physics and Technology (Vol. 4:1, pp. 84-90).
Fujifilm Synapse PACS software and an MC-R screening image-reading system were incorporated for networking and remote interpretation for 121,526 lung cancer screenings that included temporal subtraction.
From this digital imaging archive, lead author Yasuo Sasaki, MD, PhD, a radiologist at Iwate Prefectural Central Hospital in Morioka, and colleagues selected 24 abnormal studies and 270 normal cases from the historical archives. The abnormal images were initially read as suspicious. Lung cancer diagnoses were confirmed at histology.
Image quality was judged acceptable for the trial when the subtraction image had a relatively small amount of misregistration, according to the authors. From its initial evaluation, 88.4% of the temporal subtraction images in the archives were considerable acceptable.
Normal and abnormal studies were electronically shuffled for random presentation to five radiologists with more than 11 years of experience in diagnostic radiology for interpretation and assessment.
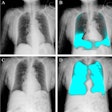
The observer performance study consisted of three reading sessions. In the first session, observers only examined the current and previous images on a workstation displaying one case at a time. In the second session, the physicians viewed current, previous, and temporal subtraction images. In the third, observers viewed current and previous images, taking into account the diagnostic results from a specific observer to simulate double readings. Three weeks elapsed between reading sessions to minimize the learning effects of repeat examination, the authors noted.
Each observer's confidence rating about the presence or absence of lung cancer on individual studies was scored on a five-point scale, ranging from 1 for "definitely absent" to 5 for "definitely present."
A receiver operator characteristics (ROC) curve analysis was performed on observer confidence and actual performance for detecting lung cancers during the three sessions.
The computerized temporal subtraction method adopted for lung cancer screening in the Iwate Prefecture was originally developed by Kunio Doi, PhD; Maryellen Giger, PhD; and Heber MacMahon, MD, at the University of Chicago in the early 1990s. It digitally subtracts ribs, spine, clavicles, and other bones known to hide the presence of suspicious lung lesions.
Average ROC curves revealed a significant improvement in lung cancer detection accuracy for interpretations performed with access to temporal subtraction images, compared to CR chest exams without temporal subtraction or simulated double-read scans.
The average area under the curve (AUC) value increased significantly, from 0.951 without temporal subtraction images and 0.890 with the double-reading method to 0.990 with the temporal subtraction method. (p = 0.028 and p = 0.002, respectively). However, statistical significance was not achieved for average AUC values for comparing interpretations of the CR chest exams without temporal subtraction and with double reading.
Four of five readers diagnosed lung cancers more accurately when they could examine the temporal subtraction images. Temporal subtraction was less helpful for ruling out cancers for normal patients.
"One possible cause for the lesser effectiveness in normal cases might be misregistration artifacts remaining in the normal lung," Sasaki and colleagues wrote. "It is necessary to reduce the artifacts on subtraction images for further improving observers' detection performance."
The exams were typically read a few seconds faster for all readers when temporal subtraction images were available, but the difference was not statistically significant.
The results suggest "that a single-reading method with previous, current, and subtraction images might replace the double-reading method with previous and current images alone in lung cancer screening," the authors concluded.