Are interventional radiologists more prone to cataracts due to medical radiation? The question was investigated at last week's Society of Interventional Radiology (SIR) conference by an eye specialist who spent the meeting peering into the eyes of attendees, looking for early signs of eye disease.
SIR's Safety and Health Committee invited Norman Kleiman, PhD, director of the Eye Radiation and Environmental Research Laboratory in the Mailman School of Public Health at Columbia University, to perform a survey during the six-day conference. He screened more than 100 interventional radiologists and control subjects, looking for symptoms and precursors to posterior subcapsular cataracts (PSC), a rare type of cataract that is usually found only in people who either took systemic steroids for long periods of time or who have been exposed to radiation.
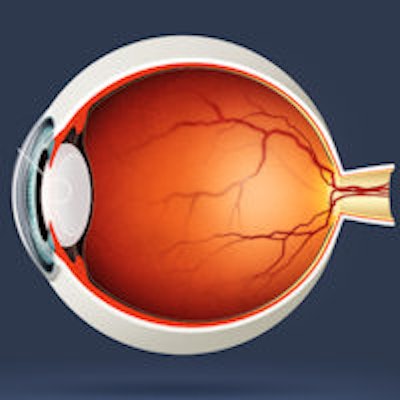
Cataracts are a condition in which the normally transparent lens of the eye becomes cloudy, eventually interfering with vision. In terms of radiation's effects, radiation damages a single layer of epithelial cells on the anterior surface of the eye's lens. These cells slowly divide and differentiate, leading to continued lens growth throughout a person's lifetime, Kleiman said.
"Transparency relies on that single layer," he said. "We think that the mature lens fiber cells become opaque due to initial radiation damage to DNA in a specific region of the overlying epithelial cell layer."
Previously, radiation-related cataracts were thought of as a deterministic event, involving the death of cells and relatively high-threshold radiation doses, he continued. "What we're learning suggests that it may be more closely linked to stochastic types of events, involving genotoxic stresses and potential mutation," he said.
Kleiman put in 11-hour days during SIR 2014 interviewing and testing interventional radiologists for his most recent study looking at the relationship between radiation exposure and this unusual kind of cataract.
The current study has a novel addition: a new way of testing for radiation-associated visual disability by measuring changes in contrast sensitivity in the eye. The approach may more closely approximate the visual tasks demanded by interventional radiology, according to Kleiman. He hypothesized that contrast sensitivity testing may provide an alternative to dilating eyes and conducting a slit-lamp exam, the current gold standard.
Contrast testing involves looking at eye test screens much like the ophthalmologists' letter chart, but with bull's eyes made with varying spacing between light and dark and varying levels of contrast. The less contrast people can see, the more opaque their lenses may be.
"We think there may be a relationship between changes in the ability to see contrast and lens opacities due to posterior subcapsular cataracts," Kleiman said. "It's another tool we can utilize to better quantitate visual disability."
In a 2004 pilot study, Dr. Ziv Haskal and Kleiman's mentor, Basil Worgul, PhD, showed that there is a correlation between how long interventional radiologists have practiced, the number of procedures they've performed, and the likelihood that they will develop posterior subcapsular cataracts. In addition, Kleiman and co-researchers published a study in February 2013 in SIR's Journal of Vascular and Interventional Radiology that estimated radiation dose delivered to cardiac cath lab personnel -- a study for which Kleiman received an award at SIR 2014.
Nearly half of the 59 interventional radiologists studied had changes in their lenses associated with PSC, and more than a third had the beginnings of opacity in the region of the lens that is affected by radiation. Several had true, potentially disabling cataracts.
At the time, radiology professionals were being told to limit their exposure to 150 mSv a year. In 2012, however, the International Commission on Radiological Protection (ICRP) recommended new, lower occupational exposure limits of 20 mSv a year averaged over five years, with no single year exceeding 50 mSv.
While the proposed exposure limits are some 20% or less of what they once were, the question of how little exposure can prompt the lens to become opaque remains unanswered. The changes are not immediate and take years to show, Kleiman said. And researchers suspect the changes are more than cell-killing.
For example, in 2008, Kleiman was part of an International Atomic Energy Agency (IAEA) team that gathered data from a group of 127 doctors, nurses, and technicians at an interventional cardiology conference; again, they found changes in the lenses associated with occupational radiation exposure. In that study, 50% of the doctors and 41% of the nurses and technologists showed evidence of posterior subcapsular lens changes characteristic of ionizing radiation exposure, compared with less than 10% of the control group.
People with the same amount of exposure can still get different results, Kleiman noted. "We suspect that individual sensitivity is a contributing factor, that genes matter in how individuals react to exposure," he said.
Data that Kleiman collected at SIR 2014 will be incorporated into a study, with the Journal of Vascular and Interventional Radiology given right of first refusal to publication.



















