A deep-learning AI model shows promise for predicting spinal curves in individuals with adolescent idiopathic scoliosis (AIS), according to a study published October 30 in the Global Spine Journal.
As a potential screening tool, the model could minimize stress and lifestyle adjustments for patients and families, as well as prevent unnecessary treatment and resource consumption, according to the researchers.
“Integrating the model’s prediction with the clinician's expertise and experience can maximize the overall accuracy of AIS progression prediction in clinical practice and can limit the influence of false positives on the patients,” wrote first author Kenneth Chu, an orthopedics student at the University of Hong Kong’s Digital Health Laboratory in China.
Scoliosis is a 3D spinal deformity, with AIS accounting for about 70% of all cases. The deformity is usually diagnosed during puberty. Treatment options depend on the severity of disease and range from observation alone to bracing and surgery.
Determining the risk of AIS progression is a complex task, the authors wrote. Moreover, most current curve progression software tools rely on 1D numerical data alone and fail to make use of subtle 2D spatial information within the spine that could be invaluable, they added.
“Such practice inevitably wastes a lot of information,” the group noted.
Thus, the researchers aimed to develop an AI neural network that can automatically predict the probability of in-brace curve progression of AIS patients at their first visit to orthopedic clinics by using both routinely collected 1D clinical data and 2D full-spine x-ray images.
The researchers recruited 463 participants between the ages of 10 and 16 who had undergone treatment with bracing orthosis and imaging prior to treatment and during follow-up visits within at least three months. They used data from 371 patients to train an existing neural network called CapsuleNet. Input included both 1D data (sex, age, weight, sitting height, standing height, arm span, Risser sign, distal radius, and ulna classification for skeletal maturity assessment) and 2D x-rays from the patients.
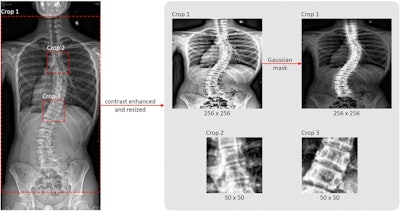 Three regions of interest (ROI) were selected and processed for training from each original radiograph. The leftmost image is the original coronal view radiograph. The original radiograph was passed through the CLAHE algorithm to enhance image brightness and contrast. The three crop boxes outlined by red dotted lines illustrate the three crops generated for model training. Crop 1 selects the ROI for the whole-spine region according to coordinates exported by AlignProCARE. Crops 2 and 3 select the ROIs for the upper and lower end vertebra of the major curvature. All ROIs were subsequently resized into 256 × 256 for Crop 1 and 50 × 50 for Crop 2 and 3. Crop 1 ROI was additionally multiplied by a Gaussian mask to amplify the signal of the vertebrae. Image courtesy of the Global Spine Journal.
Three regions of interest (ROI) were selected and processed for training from each original radiograph. The leftmost image is the original coronal view radiograph. The original radiograph was passed through the CLAHE algorithm to enhance image brightness and contrast. The three crop boxes outlined by red dotted lines illustrate the three crops generated for model training. Crop 1 selects the ROI for the whole-spine region according to coordinates exported by AlignProCARE. Crops 2 and 3 select the ROIs for the upper and lower end vertebra of the major curvature. All ROIs were subsequently resized into 256 × 256 for Crop 1 and 50 × 50 for Crop 2 and 3. Crop 1 ROI was additionally multiplied by a Gaussian mask to amplify the signal of the vertebrae. Image courtesy of the Global Spine Journal.
They then tested the model’s predictive performance in a hold-out data set from 92 patients, with AIS curve progression defined as a minimum increase of 5° in major curve Cobb angle from the time of diagnosis to any follow-up.
According to the findings, the model achieved 90% sensitivity with an overall accuracy of 73.9% in the prediction of AIS in-brace curve progression by using first-visit multidimensional data, the group wrote.
“This study utilized a modified version of the CapsuleNet model to create an AI model that predicts in-brace AIS progression risk with a high sensitivity level at 90%,” the researchers wrote.
As immediate next steps, the authors noted that more patients with AIS need to be prospectively recruited to generate a larger and complete dataset involving the accurate recording of at least the conventionally acknowledged risk factors for AIS progression and skeletal maturity indicators, along with the x-rays.
“With a more comprehensive dataset, the feasibility of this automated multidimensional approach in predicting AIS progression can be further evaluated in a prospective clinical trial,” the group concluded.
The full article is available here.