An AI model has delivered a long overdue update of pediatric bone growth predictions used in x-ray imaging to monitor scoliosis, according to a study published April 30 in Radiology.
The model’s growth curve predictions were derived from standing slot-scanning x-rays from a diverse pediatric population and proved more accurate than current methods for guiding predictions, noted lead author John Zech, MD, of New York University Langone Health in New York City, and colleagues.
“While the Anderson-Green standards remain widely used today, they are based on a sample of only 100 children whose growth was evaluated more than 60 years ago and who were not racially or ethnically diverse,” the group wrote.
Full-body biplanar slot scanning is a type of low-dose digital x-ray imaging used to monitor scoliosis. Most patients are imaged in six-month intervals for a period of one to five years. This allows clinicians to estimate growth over time and compare them with statistical averages in the Anderson-Green method, the authors explained.
Moreover, while manual measurement of femoral and tibial length on radiographs has been shown to be reliable, it is a tedious and time-consuming task, the authors added.
In this study, the authors aimed to leverage AI to improve these methods by training a convolutional neural network (CNN) model to automatically measure femorotibial length on x-ray images from a racially diverse set of pediatric patients.
The study data included 1,874 examinations from 523 pediatric patients aged 0 to 21 who underwent at least two slot-scanning radiographs in routine clinical care. Forty percent of the patients self-identified as white and not Hispanic or Latino and 60% self-identified as belonging to a different racial or ethnic group, the authors noted.
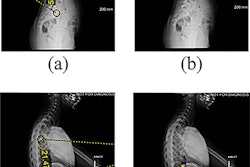
 The lower extremity measurement pipeline is illustrated using a representative slot-scanning radiograph. The AI model was trained to segment the femur and tibia: (A) the original radiograph and (B) the same radiograph showing the segmentations (boxes) produced by the model. (C) The segmentations in B were used by the model to identify the top of the femoral head, medial tibial condyle, and tibial plafond (lines). These locations were used by the model to measure the length of the femur, tibia, and lower extremity overall. Image courtesy of Radiology.
The lower extremity measurement pipeline is illustrated using a representative slot-scanning radiograph. The AI model was trained to segment the femur and tibia: (A) the original radiograph and (B) the same radiograph showing the segmentations (boxes) produced by the model. (C) The segmentations in B were used by the model to identify the top of the femoral head, medial tibial condyle, and tibial plafond (lines). These locations were used by the model to measure the length of the femur, tibia, and lower extremity overall. Image courtesy of Radiology.
The CNN model was trained to segment the femur and tibia on the x-rays and measure total leg, femoral, and tibial length, with results showing the model’s mean absolute error measurements were 0.25 cm for the femur, 0.27 cm for the tibia, and 0.33 cm for composite lower limbs.
Next, the AI measurements were used to create femoral and tibial growth curves and the researchers compared these to those derived from the Anderson-Green method.
According to the analysis, AI growth curves more accurately represented lower extremity growth in an external test set (n = 154) than the Anderson-Green method. Growth reference ranges generated using the AI model showed higher coverage probability than those generated using the Anderson-Green method (86.7% vs. 73.4%; p < 0.001), the authors reported.
Ultimately, the authors noted that this higher coverage probability demonstrates the potential value of updated standards based on a diverse population. The higher coverage may reflect greater height and greater variability in height in the modern population of children compared with the children on whom the Anderson-Green standards were based, they suggested.
“The AI model offers an easily scalable method to obtain growth data from additional patients, which may allow the creation of stratified standards that more closely fit a child’s individual growth profile,” the researchers concluded.
The full study is available here.