An AI model for x-ray imaging could help clinicians plan treatment other than spinal fusions in patients with adolescent idiopathic scoliosis, according to research published January 14 in PLOS One.
The study proposes a machine learning-based tool for planning anterior vertebral body tethering (AVBT), an emerging minimally invasive surgical treatment, noted first author Ausilah Alfraihat, a PhD student at Drexel University in Philadelphia, PA, and colleagues.
“The current model has potential to serve as a valuable clinical tool, providing insight into the optimal timing of intervention and surgical planning parameters,” the group wrote.
AVBT was approved in the U.S. in 2019 and involves implanting a flexible cord along the spine to guide spinal growth to correct deformities in adolescent patients who continue to progress despite bracing. Despite showing promise in several studies, the predictability of the procedure remains uncertain and hinges on a complex interplay of factors that are difficult to analyze clinically, the authors wrote.
Hence, the group developed a machine-learning-based algorithm that could potentially fill this gap.
The researchers included data from 91 patients with adolescent idiopathic scoliosis who underwent AVBT surgery at the Shriners Hospitals for Children in Philadelphia. For all patients, spinal x-rays were taken at six visits, from patients’ first standing x-ray to their most recent follow-up exam.
They analyzed these images, as well as demographic and surgical features associated with to identify the 11 most predictive features of subsequent AVBT corrections and trained a gradient boosting regressor (GBR) model to predict outcomes based on these features. The dataset (for all patients) was randomly split into training (80%) and testing (20%) datasets.
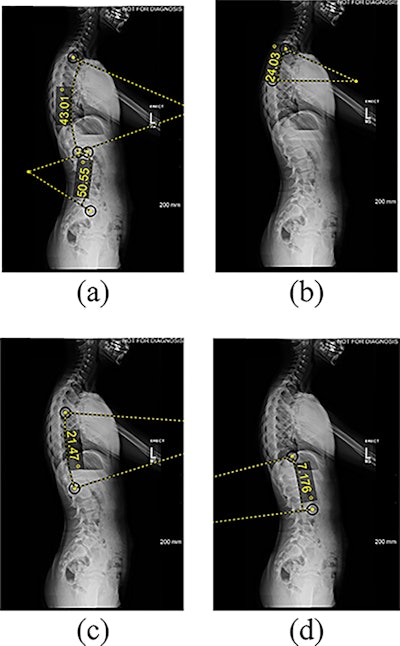 Features extracted from lateral radiographs. (a) thoracic kyphosis and lumbar lordosis (b) proximal thoracic kyphosis (c) mid-lower thoracic kyphosis (d) thoracolumbar lordosis angle measured between the superior endplate and the inferior endplate of the vertebral levels: T2-T12, L1-L5, T2-T5, T5-T12, and T12-L2. Image courtesy of PLOS One.
Features extracted from lateral radiographs. (a) thoracic kyphosis and lumbar lordosis (b) proximal thoracic kyphosis (c) mid-lower thoracic kyphosis (d) thoracolumbar lordosis angle measured between the superior endplate and the inferior endplate of the vertebral levels: T2-T12, L1-L5, T2-T5, T5-T12, and T12-L2. Image courtesy of PLOS One.
According to the findings, the AI model predicted the final Cobb angle with an average error of 6.3 ± 5.6 degrees, the authors wrote. The model also provided a prediction interval, where 84% of the actual values were within the 90% prediction interval, they added.
“The GBR model, trained on these features, predicted the final curve magnitude with a clinically acceptable margin of error,” the group wrote.
Ultimately, the authors noted that this is the first study to apply AI methods to longitudinal data from patients who underwent AVBT surgery. Significantly, the model is based on a rank-ordered list of the most predictive features associated with postsurgical curve correction, they wrote.
“This model can be used as a clinical tool to plan AVBT surgical parameters and improve outcomes,” the group concluded.
The full study can be found here.