Suture-mediated closure devices (SMCDs) are used routinely in patients undergoing treatment for peripheral vascular disease or anticoagulation. Are these devices of any value in women receiving uterine artery embolization (UAE) for symptomatic leiomyomata? At first glance, the answer is "no," according to interventional radiologists from Illinois and Oregon.
In patients with peripheral vascular disease, SMCDs have a 1% to 3% major complication rate, noted Dr. Howard Chrisman and colleagues. In comparison, that rate climbed to 5% in previous studies that have deployed SMCDs in UAE patients.
"The issue of SMCD use is controversial in the UAE population.... Traditional methods of manual compression have been defined as the standard of care, with a low major complication rate," Chrisman's group wrote. "The argument then holds that the SMCD serves only to add convenience to the procedure with no significant benefit to the patient" (Journal of Vascular and Interventional Radiology, March 2005, Vol. 16:3, pp. 347-531).
Chrisman is from Northwestern Memorial Hospital in Chicago. His co-authors are from the University of Illinois at Chicago and St. Vincent's Hospital in Portland.
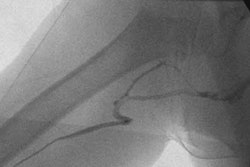
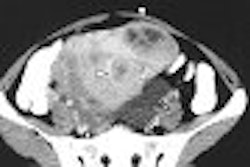
The group set out to show that using SMCDs was more than just a matter of convenience. Their patient population consisted of 342 consecutive patients who had embolization performed via a unilateral percutaneous approach through a 5.5-French sheath system. Unless there was a contraindication, primary hemostasis was attempted with the device (Closer S, Abbott Laboratories, Abbott Park, IL).
The closure was considered successful if complete hemostasis was achieved within two hours, and the patient could walk within another two hours. SMCD failure was defined as the inability to provide hemostasis postdeployment. The women were followed up at 24 hours postprocedure, at one to six months, and at one year.
SMCD closure was attempted in 328 patients (14 were deemed unsuitable candidates). Device failure occurred in eight (2.4%) of 328. Reasons for failure included the inability to capture firing needles and operator error.
Twenty-one percent of the 328 women (68) had successful SMCD closure, but presented one week later with minor anteromedial thigh pain ipsilateral to the arterial puncture site. At the time, they were treated with nonsteroidal anti-inflammatory drugs (NSAIDs), although NSAIDs have now been replaced with other oral analgesics, the authors said.
Four women (1.2%) had minor hematomas. There were no major complications such as occlusion, infection, or vessel dissection.
"The SMCD offers a shorter time to ambulation than traditional manual compression," the authors stated. "With a greater confidence in the clinical management of these patients, arteriotomy closure devices may allow for the evolution of the UAE procedure into a same-day outpatient-based treatment."
Future studies on SMCDs for UAE will need to be prospectively randomized, and should compare SMCDs to other closure methods such as hemostatic patches or collagen-mediated devices, they stated.
Chrisman will present another study on uterine fibroid embolization (UFE) at the Society of Interventional Radiology (SIR) meeting in New Orleans this week. This second study focuses on the effect of targeted marketing on an existing UFE practice. Chrisman will discuss the results of an ad campaign geared toward a particular community, which resulted in a net revenue gain of $43,000 for his institution.
By Shalmali Pal
AuntMinnie.com staff writer
March 30, 2005
Related Reading
Pregnancy possible after uterine artery embolization for leiomyomata, December 29, 2004
Uterine artery embolization for fibroids linked to adverse pregnancy outcomes, August 13, 2004
Copyright © 2005 AuntMinnie.com