Endovascular thrombectomy (EVT) is effective for stroke patients who need to be transferred from hospitals where they are diagnosed to centers capable of performing the procedure, according to a study published February 8 in JAMA Network Open.
In a clinical trial, both directly presenting patients and patients transferred to EVT-capable centers benefited from the procedure, with the results highlighting the need for rapid identification of suitable transfer patients, noted lead author Amrou Sarraj, MD, of Case Western Reserve University in Cleveland, OH.
“Patients with large ischemic core stroke have poor clinical outcomes and are frequently not considered for interfacility transfer for endovascular thrombectomy,” the group wrote.
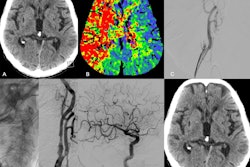
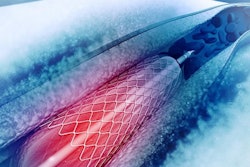
Stroke treatments are time-sensitive, with EVT proving to be a valuable approach, the authors noted, in a separate analysis published February 7 in JAMA. EVT is a minimally invasive image-guided surgical procedure that dissolves blood clots and thus restore blood flow to prevent further brain damage.
In this study, the researchers conducted a subgroup analysis using data from a recently completed clinical trial that compared EVT to standard medical management at 31 centers across North America, Europe, Australia, and New Zealand. In the trial, hospitals without neurointerventional teams transferred participating patients to EVT-capable centers.
The group culled data on these patients and assessed EVT treatment effects, as well as associations between transfer times and neuroimaging changes.
Out of 352 enrolled patients (median age, 66.5 years old), a total of 211 patients were transfers, of whom 108 (51.2%) received EVT, while 141 patients presented directly, of whom 72 (51.1%) received EVT. All patients had a large ischemic core diagnosed by either noncontrast CT and/or CT perfusion or MRI diffusion-perfusion imaging within 24 hours of the time they were last known well. The median transfer time for patients was 178 (136-230) minutes.
According to the analysis, both directly presenting and transferred patients had better clinical outcomes after 90 days with EVT compared with medical management, the authors wrote. Specifically for transfer patients, they found the benefits of EVT favored patients with low Alberta Stroke Program Early CT Scores (ASPECTS), a CT scoring system for identifying early tissue damage.
However, the association of EVT with better functional outcomes was numerically better in patients presenting directly to EVT-capable centers, the group added.
“Patients with transfer times less than 3 hours demonstrated better functional outcomes with EVT [compared to medical management], whereas treatment effect estimates were lower but still favored EVT in those with longer transfer time,” the researchers wrote.
Ultimately, implementation of the findings could have clinical implications, given that a significant proportion of patients with stroke present to non–EVT-capable centers, the authors wrote. These centers provide initial treatment and then coordinate patient transfers to EVT-capable centers after neuroimaging to evaluate the need for a higher level of care.
“These findings may impact stroke systems of care infrastructure, highlighting the need for rapid identification of patients suitable for transfer and expedited transport and reperfusion on arrival,” the researchers concluded.
The full article is available here.