The benefits of endovascular thrombectomy in patients with acute basilar artery occlusion are sustained at long-term follow-up, according to a study published August 26 in JAMA Neurology.
In an analysis of outcomes of a large clinical trial, researchers found that “excellent” outcomes increased between 90 days and one year in patients who underwent the procedure, but not in patients who received only intravenous thrombolytics, antiplatelet drugs, or anticoagulants (the three of which currently represent best medical treatment).
“Patients in the thrombectomy group had a greater likelihood of achieving an excellent outcome and functional independence compared with those in the control group,” wrote lead author Rui Li, MD, PhD, of the University of Science and Technology of China in Hefei.
Acute basilar artery occlusion is a rare but potentially catastrophic condition. It occurs when the basilar artery at the base of the brain becomes blocked, with up to 68% of patients dying or remaining severely disabled.
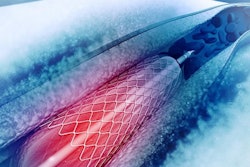
Endovascular thrombectomy is a minimally invasive image-guided surgical procedure that can be used to dissolve blood clots in these patients, and thus restore blood flow to prevent further brain damage. The intervention has been shown to improve functional outcomes at 90 days, yet information on long-term outcomes is still unclear, the authors noted.
To that end, they analyzed data among 330 patients who had one-year follow-up in a multicenter, population-based study conducted at 36 comprehensive stroke sites in China. Patients with acute basilar artery occlusion who underwent the procedure within 12 hours of symptom onset were included.
To determine outcomes, the researchers used scores on the modified Rankin Scale (mRS), a 6-point scale that measured the degree of disability in patients, including functional independence (mRS score 0 to 2), excellent outcome (mRS score 0 to 1), and level of disability (distribution of all mRS scores).
According to the findings, an mRS score of 0 to 3 (no symptoms to moderate disability) at one year was achieved by 99 of 222 patients (44.6%) in the thrombectomy group compared to 21 of 108 (19.4%) in the control group.
In addition, excellent outcome (mRS scores of 0 to 1) at one year compared with 90 days increased in the thrombectomy group (62 of 222 [27.9%] vs. 45 of 226 [19.9%]) but not in the control group (9 of 108 [8.3%] vs. 9 of 114 [7.9%]), resulting in a “magnified treatment benefit,” the researchers wrote.
“Outcomes between 90 days and one year in the thrombectomy group reflects that stroke recovery may continue well beyond the first three months among survivors of severe acute ischemic stroke,” the group noted.
Ultimately, the findings may assist clinicians and patients in the decision-making process, the group suggested. Clinicians can leverage these results to highlight the potential of endovascular thrombectomy for improving long-term functional recovery, they wrote.
“The long-term benefits in terms of functional independence, survival, and quality of life are essential for patients and caregivers to appreciate the value of endovascular thrombectomy,” the group concluded.
The full study can be found here.