UCLA neuroscientists used PET to determine the effectiveness of paroxetine (Paxil) in treating obsessive compulsive disorder (OCD) versus major depression. The study, in the March 2003 American Journal of Psychiatry, compares neurobiological predictors of response to the same treatment of these disorders.
While the two disorders are quite different clinically, they often coexist in patients, said Dr. Sanjaya Saxena, director of the UCLA Neuropsychiatric Institute’s OCD research program. He also is an associate professor-in-residence of psychiatry and biobehavioral sciences at UCLA’s David Geffen School of Medicine.
Two-thirds or more of patients with OCD experience major depression at some point in their lives. And about a third of patients with OCD have major depression at a given time. Likewise, OCD symptoms are sometimes seen to a mild degree in depressed patients.
Saxena said the intent was to find out about the similarities and differences between OCD and major depression.
"Both are common, chronic, debilitating neuropsychiatric disorders that have a pretty high rate of comorbidity. We wanted to find out if they were biologically similar, because serotonin reuptake inhibitors (SRIs) can be used to treat both disorders. We wanted to find out whether those treatments had the same or different mechanisms of actions when treating OCD versus major depression."
Saxena said investigators also wanted to determine whether pretreatment brain activity patterns that predicted response were similar or different, and whether the disorders have different neural substrates for response to a given agent.
Seventy-one subjects completed the study -- 27 patients with OCD alone, 27 with major depressive disorder alone, and 17 with concurrent OCD and major depressive disorder.
"We needed to study a large group of people with depression alone, with OCD alone, and a third group of people with both disorders to try and tease apart some of these differences and similarities on a neurobiological level," he said.
Image acquisition
Each subject received 5-10 mCi of FDG while in a supine position with eyes and ears open. Subjects were closely monitored to make sure that they remained awake and lay still without moving or talking during the 40-minute FDG uptake period. No cognitive task was given.
PET was performed with two ECAT III 831 (15 transverse sections spaced 6.75 mm apart, with a 6-mm in-plane spatial resolution, acquired at an angle parallel to the canthomeatal plane) in the first 38 subjects, and the EXACT HR1 961 (both scanners by Siemens Medical Solutions-Nuclear Medicine Group , Hoffman Estates, IL) (47 transverse sections spaced 4.0 mm apart, with a 3.6-mm in-plane spatial resolution) in the next 33 subjects (American Journal of Psychiatry, March 2003, Vol.160:3, pp.522-532).
Each subject also received an MRI scan of the brain during the treatment period. The images were obtained using a double-echo sequence (proton density and T2-weighted images, TR=2000 to 2500 msec, TE=25 to 30 msec and 90 to 110 msec, 24-cm field of view, 3-mm slices with no separation). A neuroradiologist reviewed all of the MRI scans. Any prospective subject with MRI evidence of structural central nervous system (CNS) lesions was excluded from the study.
Conclusions
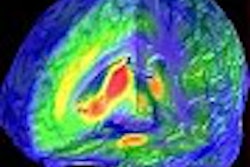
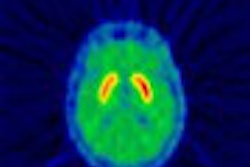
According to the results, improvement of OCD symptoms was significantly correlated with higher pretreatment glucose metabolism in the right caudate nucleus. However, improvement of major depressive disorder symptoms was significantly correlated with lower pretreatment metabolism in the amygdala and thalamus, and with higher pretreatment metabolism in the medial prefrontal cortex and rostral anterior cingulate gyrus.
The findings suggest that although both OCD and major depressive disorder respond to SRIs, the two syndromes have different neurobiological substrates for response, Saxena said. Elevated activity in the right caudate may be a marker of responsiveness to antiobsessional treatment, while lower-right amygdala activity, and higher midline prefrontal activity, may be required for response of depressive symptoms to treatment.
"We’ve shown that the disorders are very different in a variety of ways, perhaps more than people realized," he said. "They may respond to the same drug, but they have different brain changes when they respond to the drug and they also have different patterns of pretreatment brain activity that seem to be responsible for treatment responsiveness."
Saxena said a lot of people would like to use PET as a diagnostic tool, but there is a great deal of overlap in the patterns of brain abnormalities between different groups. In addition to the cost of screening large number of patients, PET doesn’t have the sensitivity and specificity for most neuropsychiatric disorders, he said. The only neuropsychiatric disorder for which PET can really be used as a diagnostic tool at present is Alzheimer’s disease, where there are characteristic brain abnormalities that are quite distinct from those seen in normal controls.
The goal might be to screen patients with PET to help us tailor the eventual care, Saxena said, to find out whether they have a brain activity pattern that has been associated with response to a particular drug class or to cognitive behavioral therapy for OCD. In depression it might be used to predict response to one of several different kinds of antidepressants that can be effective -- where now it’s a process of trial and error. He said that if researchers can find a set of patterns sensitive and specific enough, it save costs in the long run by saving patients unnecessary trials of medications.
By Robert BruceAuntMinnie.com contributing writer
April 2, 2003
Related Reading
MR spectroscopy reveals reduced neuronal viability in ADHD kids, March 18, 2003
Functional MRI shows effects of antidepressants, February 28, 2003
fMRI reveals secrets of better memory, January 13, 2003
MRI shows differences between adults with ADHD, controls, December 9, 2002Copyright © 2003 AuntMinnie.com