When a severe imbalance of insulin levels is confined to a limited section of a baby's pancreas, PET has shown to be extremely accurate in locating the abnormality at the Children's Hospital of Philadelphia (CHOP) and the University of Pennsylvania School of Medicine.
Congenital hyperinsulinism is the most common cause of hypoglycemia in infants and children and is caused by mutations that damage the insulin-secreting beta cells in the pancreas. Focal disease can be cured by surgical removal of the focal lesions. In diffuse disease, surgeons may remove nearly the total pancreas, but that leaves the child at risk for later diabetes.
Affected newborns will show signs of hypoglycemia in the first day or two after birth. About half require surgery, because the condition cannot be controlled medically. Over the last 10 to 15 years, it has been increasingly recognized that of the children who need surgery, between 50% and 60% can be cured through the procedure.
CHOP research
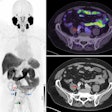
Researchers reviewed 24 newborns at CHOP from December 2004 and November 2005. Using the radioactive compound 18F-fluoro-L-dihydroxyphenylalanine, or [18F]-DOPA, the team correctly diagnosed focal or diffuse hyperinsulinism in 23 of the 24 cases. [18F]-DOPA binds to the lesions, which become visible to the naked eye on a body scanner. In 11 patients with focal hyperinsulinism, the technique located the abnormal lesions in every case.
“Without the PET scan, the surgeon is pretty much blind when he operates on the pancreas, because the lesions are not usually visible or palpable," Stanley said. "It is a hit-or-miss process, taking pieces of the pancreas out and hoping you have gotten the lesion."
Satellite lesions in the pancreas also have been discovered through the PET scan.
Hyperinsulinism can be difficult to manage, Stanley said, especially if it is a severe case of hypoglycemia, which can cause seizures, brain damage, permanent retardation, and, potentially, death. He added that the rate of brain damage in recent years has been as high as 40%. Babies must remain in a neonatal intensive care unit and cannot be sent home until the condition is under control.
Compact scanner
CHOP uses a standard PET brain scanner at the facility next to the hospital. Susan Becker O'Rourke, RN, nurse coordinator of CHOP's Congenital Hyperinsulinism Center, said their reliance on a dedicated scanner is because the brain scanner is not in use as much as the facility's conventional PET scanner. The compact PET brain scanner can accommodate children as old as 15 to 18 months.
“When we found the focal lesions, it was very effective in helping us locate exactly where in the pancreas the surgeon needed to look for the surgery,” she said.
The dose of radiation the newborn receives from the PET scan is less than 1 millicurie, O'Rourke noted. The half-life of fluoradopa also is very short, so exposure is minimal and it excreted through the urine quickly. The PET scan itself takes approximately 90 minutes. Newborns are kept under general anesthesia to eliminate unnecessary movement that would adversely affect the images.
Graduation day
Before newborns are released from the hospital, CHOP conducts what Stanley described as a “graduation test.” Babies fast for as long as 18 hours to prove there are no signs of hyperinsulinism. If blood sugar remains normal during that time, doctors know the baby is cured. It is a "much more definitive test than going back and repeating the PET scan,” he added.
The babies that are cured do not return to CHOP, as no additional follow-up is required. "They are seen once more a month or two after discharge by a surgeon to check and make sure there are not post-surgical issues," Stanley said. "With this particular condition, we’re not worried about re-growth; it is not a cancer. If we can get all of the focal lesion by surgery, it’s a home run.”
Many newborns who have the diffuse disease are still somewhat hypoglycemic after surgery and require continued follow-up. Not all infants with the diffuse disease will survive.
Since commencing the congenital hyperinsulinism PET program in February 2004, CHOP's Congenital Hyperinsulinism Center -- the only facility of its kind in the U.S. -- has handled 69 cases from around the world, including the U.S., Canada, Saudi Arabia, South America, and Iceland.
Worldwide need
“Babies have come here because the ([18F]-DOPA) PET scan procedure is not available in very many places," Stanley said. "The [18F]-DOPA is not an FDA-approved marketed isotope. It has to be synthesized the morning of the procedure at the university’s cyclotron facility.”
The technique is conducted under an FDA investigational new drug (IND) submission.
As for the future, CHOP recently installed a PET/CT scanner and soon will move the congenital hyperinsulinism program to its facility. The PET/CT scanner will co-register scans from the two modalities into one image. To date, physicians have had to perform separate CT and PET scans and merge the images.
“Having the PET/CT combination will make the visualization and localization better," Stanley said. "It also simplifies issues about having an anesthesiologist available to manage. We’ll have control of the facility here.”
By Wayne Forrest
AuntMinnie.com staff writer
August 7, 2007
Related Reading
PET scan can localize insulinoma and beta-cell hyperplasia in adult patients, May 10, 2007
Hyperglycemia associated with increased cancer risk, March 16, 2007
Study: PET accurate for newborns' pancreatic defects, January 30, 2007
PET added to lymphoma assessment guidelines, January 23, 2007
Leukemia, lung cancer risk higher in non-Hodgkin's lymphoma survivors, May 9, 2006
Copyright © 2007 AuntMinnie.com