Healthcare insurance companies should value PET imaging and its cost-effective contributions to patient outcomes rather than view the modality as too expensive and unworthy of reimbursement, according to an editorial in the December issue of the Journal of Nuclear Medicine.
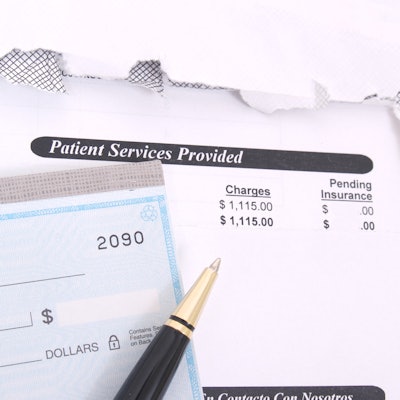
A trio of authors from the David Geffen School of Medicine at the University of California, Los Angeles (UCLA) suggest that insurance payors taking cost-savings measures should focus on labor and goods, such as administrative costs and pharmaceuticals, instead of denying coverage for PET, a modality that has proven its proficiency in patient diagnoses (JNM, December 2019, Vol. 60:12, pp. 1657-1658).
"The nuclear medicine community has at times been very successful in turning the tide (National Oncologic PET Registry). Yet, we have not completely overcome the industry's Pavlovian resistance reflex against PET imaging," wrote lead author Dr. Johannes Czernin, JNM editor in chief, and colleagues. "We have (reluctantly) accepted reimbursement cuts, limitations on clinical indications, vague coverage language, and evasive insurance behavior. We have tolerated endless peer-to-peer discussions with 'experts' who are poorly informed about imaging technologies."
As one example of inadequate coverage and company inconsistency, the authors cited an August 2019 study in which editorial co-author Dr. Jeremie Calais and colleagues compared PET imaging with gallium-68 PSMA PET/CT against fluciclovine (Axumin, Blue Earth Diagnostics) for detecting early biochemical prostate recurrence. The study hit a minor speed bump when researchers were forced to exclude 19 subjects (20%) whose insurance coverage was denied for the fluciclovine-PET scan, even though the tracer received clearance from the U.S. Food and Drug Administration (FDA) in 2016 and reimbursement approval from the U.S. Centers for Medicare and Medicaid Services (CMS) in 2017.
"Aetna considers fluciclovine-PET experimental and investigational for prostate cancer and for all other indications because of insufficient evidence," the authors noted. Conversely, Blue Shield does reimburse for fluciclovine-PET scans, deciding that the scans "may be medically necessary for evaluating suspected or biochemically recurrent prostate cancer after primary treatment to detect small-volume disease in soft tissues."
One primary misconception is that PET/CT is expensive. The fact is that the hybrid modality "accounts for only a small portion of cancer care and cancer imaging costs," the authors added.
"We thus have a toxic scenario: PET has the reputation of being expensive, an odd notion given that standard-of-care PET/CT studies include whole-body PET and diagnostic-quality CT studies," Czernin and colleagues wrote. "Nevertheless, this perception has led to further limits in FDG-PET use (lifetime cap for Medicare patients; tedious and frustrating preauthorization procedures for non-Medicare patients)."
If healthcare insurance firms such as Aetna, Blue Cross/Blue Shield, and CMS "pride themselves in promoting precision medicine," they should use PET's ability to determine early treatment responses to cancer and other diseases "without limitations," the authors concluded. "Consistently covering Food and Drug Administration-approved diagnostic tests, such as fluciclovine-PET, would go a long way toward improved patient care (precision oncology)."
Disclosure
JNM is independent of the Society of Nuclear Medicine and Molecular Imaging (SNMMI). The opinions expressed in the editorial do not necessarily reflect the position of the SNMMI.