PET/CT significantly outperformed CT alone in predicting treatment response in patients with relapsed or refractory Hodgkin's lymphoma when treated with the cancer drug nivolumab, according to multicenter results published April 14 in Radiology.
Initial PET/CT scans correctly reclassified complete response 6.5 times more often than CT alone and twice as often when patients underwent follow-up scans some two months later.
"If confirmed by further prospective studies, then our findings suggest that these techniques could guide risk-adapted strategy," wrote the authors, led by Dr. Fatima-Zohra Mokrane, PhD, from Centre Hospitalier Universitaire de Toulouse in France.
PET/CT is considered the go-to modality when evaluating the response and prognostic outcome of cancer patients to nonimmune treatment. An accurate early assessment of response by PET/CT "guides treatment de-escalation in patients with PET findings negative for Hodgkin's lymphoma and treatment intensification in patients with PET findings positive for Hodgkin's lymphoma," the researchers noted.
However, PET/CT's performance in determining the efficacy of immunotherapy -- that is, using a patient's own immune system to fight the cancer -- compared with CT alone is not well documented. To help fill that void, researchers from 34 institutions in France, the U.S., and China compared the technology's prowess in determining early response with treatment using nivolumab (Opdivo, Bristol-Myers Squibb) and overall survival in patients with relapsed or refractory Hodgkin's lymphoma.
The retrospective study included 45 patients (median age, 37 years; range, 18-77 years) who underwent PET/CT and CT imaging between a median of 2 months (range, 1.7-3.7 months) after nivolumab therapy. Of those subjects, 36 people (80%) also underwent follow-up scans a median of 6.7 months (range, 3.9-7.4 months) after nivolumab treatment. There were 11 patients (24%) who died a median follow-up of 24 months (range, 3-34 months) after treatment.
Based on initial scans, CT confirmed either a complete or partial response to therapy in 20 patients (44%), compared with PET/CT, which confirmed a complete or partial response to therapy in 25 patients (56%). Despite PET/CT and CT alone showing "substantial agreement" on treatment, the authors noted, PET correctly reclassified CT results for 11 patients (24%) as having a complete metabolic response to therapy, compared with only two patients on CT (4%) (p < 0.001).
In the review of follow-up scans, CT's ability to accurately determine complete therapy response increased to six (17%) of 36 surviving patients, but the modality still significantly lagged behind PET, which detected additional complete metabolic responses and progressive metabolic diseases and reclassified 11 patients (31%).
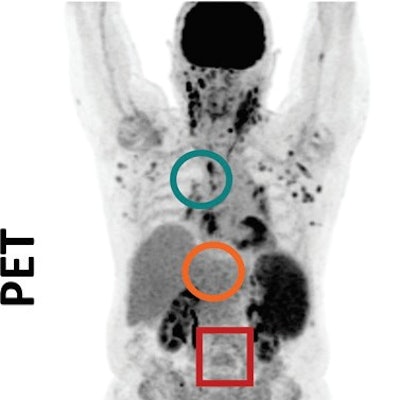
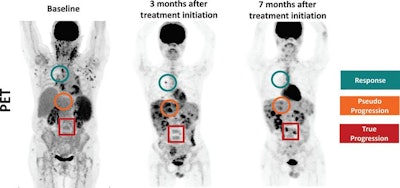 PET images show example of partial hepatic pseudoprogressive lesions at the initial PET/CT scan of a 22-year-old male. Lesions size and metabolism progressed as the patient was treated with nivolumab. The lesions did not significantly alter response evaluation, as the patient experienced mixed response with true-progressive, pseudoprogressive, and complete-responding lesions. Images courtesy of Radiology.
PET images show example of partial hepatic pseudoprogressive lesions at the initial PET/CT scan of a 22-year-old male. Lesions size and metabolism progressed as the patient was treated with nivolumab. The lesions did not significantly alter response evaluation, as the patient experienced mixed response with true-progressive, pseudoprogressive, and complete-responding lesions. Images courtesy of Radiology.As one might expect, both CT and PET/CT were able to predict an excellent probability of two-year overall survival for all patients who experienced a complete response to treatment. Given this finding, the researchers suggested "treatment de-escalation" be considered for these patients after a promising initial PET/CT or CT scan to decrease the chances of treatment-related toxicity and to reduce costs to the patients.