FDG-PET/CT can help identify lung cancer patients prior to surgery who may be at higher risk for developing advanced disease, according to research published July 25 in Seminars in Thoracic and Cardiovascular Surgery.
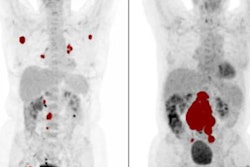
A group of researchers at Niigata University in Japan analyzed radiotracer uptake in early-stage lung cancer patients who had tumors removed and found patients with higher maximum standardized uptake values (SUVmax) had more advanced disease after three years. The study finding could help doctors devise earlier, more effective treatment strategies, according to the team.
"The SUVmax for the primary tumor should be considered when deciding treatment strategy in early-stage lung adenocarcinoma," wrote lead author Dr. Terumoto Koike, PhD, and colleagues.
Lung cancer is the most commonly diagnosed cancer and the leading cause of cancer-related death in the world. FDG-PET/CT imaging is widely used in surgical staging of tumors. Also, by studying removed tumor samples, doctors gain clinical-pathological information about the cancer in features strongly associated with poorer outcomes.
In this study, Koike and colleagues explored whether high SUVmax prior to surgery correlates with advanced disease and high-risk features in surgically removed tumors in patients with clinical stage 0–IA lung cancer.
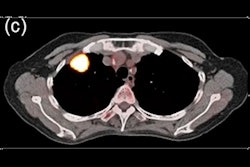
The group noted that the study began July 15, 2015, the date FDG-PET/CT was introduced at their hospital. The researchers analyzed imaging and laboratory characteristics from tumors in 291 consecutive patients with clinical stage 0–IA lung cancer who underwent FDG-PET/CT and surgery at Niigata University Hospital through March 2021. The median age of patients was 70, with 142 males and 149 females. Imaging was performed using a dedicated PET/CT scanner acquired in a continuous-bed-motion mode (Biograph mCT Flow, Siemens Healthineers).
Disease-free survival (DFS) was calculated by either the date of surgery to the date of detection of the first recurrence, by any cause of death, or by the last follow-up visit.
Patients with an SUVmax of 3.2 or higher had a significantly higher prevalence of high-risk pathological tumor features, the researchers found. At three years after surgery, only two of the 169 patients with an SUVmax lower than 3.2 showed more advanced disease and high-risk features, compared with 53 of the 122 patients with an SUVmax of 3.2 or more.
The DFS was 92.5% for patients with an SUVmax less than 3.2 and 76.5% for those with an SUVmax greater than or equal to 3.2.
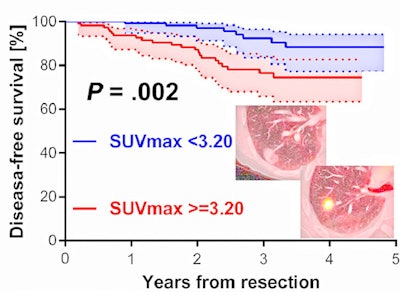 Disease-free survival (DFS) curves according to the maximum standardized uptake value (SUVmax) on FDG-PET. Solid lines represent the observed probability curve, and dotted lines represent the 95% confidence interval (CI). The three-year DFS rates in patients with an SUVmax lower than 3.2 (blue line) and those with an SUVmax of 3.2 or higher (red line) were 92.5% and 76.5%, respectively. Image courtesy of Seminars in Thoracic and Cardiovascular Surgery.
Disease-free survival (DFS) curves according to the maximum standardized uptake value (SUVmax) on FDG-PET. Solid lines represent the observed probability curve, and dotted lines represent the 95% confidence interval (CI). The three-year DFS rates in patients with an SUVmax lower than 3.2 (blue line) and those with an SUVmax of 3.2 or higher (red line) were 92.5% and 76.5%, respectively. Image courtesy of Seminars in Thoracic and Cardiovascular Surgery."A higher SUVmax for the primary tumor correlated with more advanced disease and high-risk features of patients with clinical stage 0–IA lung adenocarcinoma," the group wrote.
Most patients with a lower SUVmax did not develop more advanced disease and high-risk features and had excellent postoperative outcomes, the researchers added. They suggested, moreover, that patients with a high SUVmax may not be suitable for treatments other than surgery, such as stereotactic ablative radiotherapy and radiofrequency ablation, and rather may be more appropriate candidates for preoperative invasive mediastinal assessment and systemic mediastinal lymphadenectomy.
"We believe that our data strongly support an association between the SUVmax for the primary tumor on FDG-PET/CT, which was obtained via objective and semiquantitative analysis, and postoperative pathological metastasis and involvement in lung adenocarcinoma," Koike et al concluded.