PET/CT imaging can help predict survival early after the start of chemotherapy in patients with pancreatic cancer, according to a study in the August 5 issue of the Journal of Nuclear Medicine.
A team of researchers led by first author Dr. Matthias Benz performed F-18 FDG PET/CT whole-body scans in patients with pancreatic ductal adenocarcinoma (PDAC) before and during treatment with chemotherapy. The group found changes in tumors detected in the PET/CT imaging four weeks after initiation of first-line treatment predicted overall survival in patients.
By understanding correlations between chemotherapy response and patient survival, clinicians hope to better manage treatment approaches.
"[F-18] FDG PET allows survival predictions early after the initiation of first-line therapy in patients with PDAC and might therefore potentially serve as early interim endpoint biomarker in research and clinic," wrote Benz, assistant professor at the University of California, Los Angeles, and colleagues.
Current imaging approaches for determining whether chemotherapy is working in patients with pancreatic cancer focus on the size of tumors. However, these methods, which include CT and MRI, are less than perfect for discriminating between viable tumors, desmoplastic stroma, and dead scar tissue, even after successful therapy, according to the authors. The researchers hypothesized that F-18 FDG PET imaging could offer better early and late interim biomarkers for determining overall survival in comparison to changes in tumor size.
The study included 23 patients with biopsy-proven pancreatic cancer who underwent imaging exams between February 2013 to February 2019. The patients had exams at baseline, at 3.6 weeks, and at 11.4 weeks after the start of treatment and were then tracked for further clinical data and overall survival. Twenty-three deaths occurred during a median follow up period of 14 months.
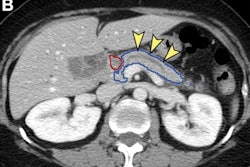
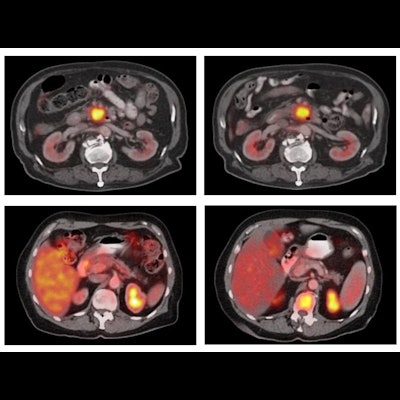
Cutoffs for early and late metabolic tumor response were determined by mPERCIST (≥ 30% decrease in tumor SUVmax), while the cutoff for early size response was based on tumor decrease (≥ 20%). Late size response was defined according to RECIST1.1 (≥ 30% decrease in tumor size). Three nuclear medicine physicians who interpreted the images were aware of the pancreatic cancer diagnosis but blinded to the treatment regimen and other clinical and outcome data, the team noted.
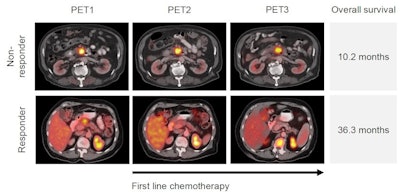 Image courtesy of the Journal of Nuclear Medicine.
Image courtesy of the Journal of Nuclear Medicine.Six of 23 patients (26%) were defined as early metabolic responders and seven of 23 (30%) as early radiographic responders. Median overall survival was 36.2 months in early metabolic responders and 25.4 months in early radiographic responders.
Ten out of 21 patients (48%) and seven out of 21 (33%) were defined as late metabolic and radiographic responders. Median overall survival was 27.4 months in late metabolic responders and 58.2 months in late radiographic responders.
"Metabolic response assessed four weeks after initiation of first-line chemotherapy served as an early interim imaging biomarker of overall survival in patients with PDAC," the researchers wrote.
Ultimately, the patient cohort was too small for a strong statistical analysis, and Benz and colleagues suggested that a chemotherapy response classification system that considers both metabolic and radiographic responses merits further investigation.
"[F-18] FDG PET may serve as an early interim imaging biomarker (~ at 4 weeks) for evaluation of response to first-line chemotherapy in patients with PDAC," they concluded.