PET/MRI can identify the brain lesions causing seizures in patients with drug-resistant epilepsy when standard approaches fail, according to research published November 20 in Epilepsy Research. The findings may offer hope for patients for whom surgery is often the only treatment option.
A French group found that PET/MRI with a hybrid scanner was better at identifying target lesions for surgery in epilepsy patients when compared with either approach alone or when PET and MRI images were fused (PET+MRI) together. The approach improved the outcomes of surgery in 40% of patients.
"Simultaneous acquisition of PET and MRI improved the detection of epileptogenic lesions, allowing a higher proportion of successful surgery and simplifying the presurgical workup, even in the more complex cases," wrote first author Dr. Anthime Flaus of Paris-Saclay University and colleagues.
Approximately one-third of people with epilepsy develop a version of the condition in which medicine can't control seizures. Most patients eventually undergo surgery to remove the lesions -- called focal cortical dysplasias (FCDs) -- suspected of causing the seizures.
FCDs can be difficult to identify even using the most optimal MRI protocols, according to the researchers. Adding PET scans and fusing the images with MRI scans improves the detection of lesions, yet this approach is also suboptimal since it requires imaging to be performed separately and on different machines.
Hybrid PET/MRI scanners are relatively new and whether they offer additional value for surgical decision-making remains to be established, the researchers wrote.
In the current study, the French group retrospectively compared fused imaging from separate MRI and PET scans in 25 patients with drug-resistant epilepsy who also then underwent scans on a hybrid PET/MRI scanner at their hospital between 2017 and 2020.
Two readers -- a junior nuclear medicine physician and a senior neuroradiologist with experience in PET and epilepsy imaging -- assessed the imaging, while the clinical impact on surgical strategy and outcome was assessed independently.
The group found that MRI was initially considered negative in 21 patients. Standalone PET identified abnormalities in 19 cases (76%) and detected four additional structural lesions when fused with MRI imaging. Compared with the fused PET and MRI scans, hybrid PET/MRI sensitivity increased by 13% and identified new structural lesions (mainly focal cortical dysplasias) in six patients (24%).
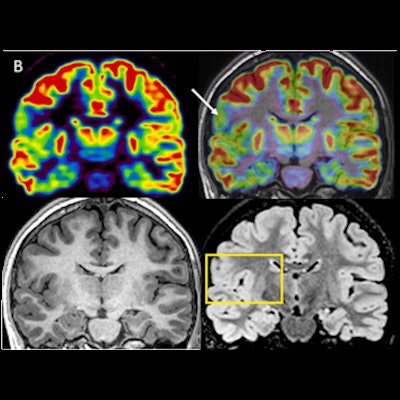
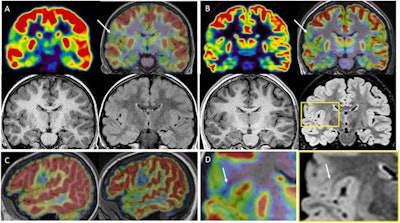 Comparison between PET+MRI (A) and PET/MRI (B); axial and coronal plane, PET alone and co-registered on MRI. The subject is a 17-year-old female with drug-resistant epilepsy since the age of 2 years; nocturnal frontal seizures (3 times per night), left frontotemporal ictal onset, negative MRI (3 tesla). Her first PET examination co-registered on MRI at 11 years considered negative; PET/MRI six years later, showing a focal hypometabolism involving the posterior part of the left orbitofrontal cortex, relative involvement of the adjacent cortex (gyrus rectus, anterior part of the left inferior frontal gyrus) and the temporal pole. This hypometabolism was retrospectively found on the previous PET but remained inconclusive. Note that the co-registration was imperfect on this examination, whereas it was almost perfect on the PET/MRI, allowing a better confidence for the visual analysis. The patient was operated on without invasive monitoring despite a negative MRI scan. Surgery was based on a PET/MR guided cortical resection, including the hypometabolic orbitofrontal cortex and the adjacent inferior frontal gyrus, in front of Broca area. FCD type 2 A was found in the cortical specimen. The patient has been seizure-free for two years and the use of antiepileptic drugs greatly reduced. Image courtesy of Epilepsy Research.
Comparison between PET+MRI (A) and PET/MRI (B); axial and coronal plane, PET alone and co-registered on MRI. The subject is a 17-year-old female with drug-resistant epilepsy since the age of 2 years; nocturnal frontal seizures (3 times per night), left frontotemporal ictal onset, negative MRI (3 tesla). Her first PET examination co-registered on MRI at 11 years considered negative; PET/MRI six years later, showing a focal hypometabolism involving the posterior part of the left orbitofrontal cortex, relative involvement of the adjacent cortex (gyrus rectus, anterior part of the left inferior frontal gyrus) and the temporal pole. This hypometabolism was retrospectively found on the previous PET but remained inconclusive. Note that the co-registration was imperfect on this examination, whereas it was almost perfect on the PET/MRI, allowing a better confidence for the visual analysis. The patient was operated on without invasive monitoring despite a negative MRI scan. Surgery was based on a PET/MR guided cortical resection, including the hypometabolic orbitofrontal cortex and the adjacent inferior frontal gyrus, in front of Broca area. FCD type 2 A was found in the cortical specimen. The patient has been seizure-free for two years and the use of antiepileptic drugs greatly reduced. Image courtesy of Epilepsy Research.In addition, hybrid PET/MRI resulted in changes in surgical decisions for 10 patients (40%), consisting of avoiding invasive monitoring in six patients and modifying the planning in four others, the researchers found.
"Hybrid PET/MR may improve the detection of epileptogenic lesions, allowing to optimize the presurgical workup and to increase the proportion of successful surgery even in the more complex cases," the study authors stated.
Ultimately, the clinical use of hybrid PET/MRI technology is currently limited due to its higher cost, the researchers wrote. However, the modality is becoming increasingly available since its introduction about 10 years ago. They noted there are now three PET/MRI systems in the Paris area.
"We believe that [PET and MRI] acquired in a single session on a hybrid system would be helpful for the presurgical evaluation of epileptic patients, especially in case of previous negative imaging findings," the researchers concluded.