A feasibility study could revive interest in SPECT seizure imaging to help neurosurgeons guide brain surgery in epilepsy patients, according to a team in Switzerland.
The researchers leveraged what they described as an untapped opportunity that allowed them to perform SPECT just seconds after triggering seizures, with the imaging visualizing brain regions associated with language difficulties in three patients, noted lead author Sabry Barlatey, MD, PhD, of University Hospital of Bern, and colleagues.
“We show that triggering of seizures with direct electric stimulation for ictal SPECT imaging is convenient, spares resources, and can be clinically useful,” the group wrote. The article was published January 11 in the Journal of Nuclear Medicine.
Delineating brain areas of seizure onset and propagation is a necessary step toward tailoring surgery for focal epilepsy. Ictal SPECT is a key method to capture complete views of propagating seizures by imaging areas of parenchymal hyperperfusion, they explained. However, the unpredictable timing of fleeting seizures in patients renders ictal SPECT acquisitions logistically challenging, they noted.
“Most epilepsy centers, including ours, abandoned this informative technique,” the group wrote.
However, patients with epilepsy often undergo stereotactic electroencephalography (sEEG) monitoring. This involves placing electrodes directly into specific regions of the brain to identify the origin of seizures. sEEG is also used to trigger patient-typical seizures using direct electric stimulation, and this helps neurosurgeons determine whether intervention is a viable option for seizure control.
“We used this untapped opportunity to image planned seizures,” they wrote.
Within a few attempts over three to eight minutes, the researchers successfully triggered seizures in three participants and in each case, they injected technetium-99m (Tc-99m) HMPAO radiotracer within nine to 12 seconds of seizure onset. This was followed by SPECT imaging within 21-39 minutes.
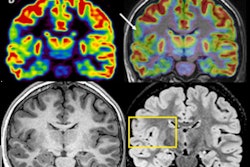
 Schematic of triggered ictal SPECT and data processing. (A) Previously screened and selected sEEG bipolar contact is stimulated to trigger patient-typical seizure. Directly after seizure onset, confirmed through sEEG signals and semiology, systemic bolus of radiotracer (Tc-99m HMPAO) is administered. Planned SPECT is acquired within less than one hour. (B) Raw data processing from left to right (dataset from participant three as example). Postimplantation CT and preimplantation T1-weighted MRI are coregistered for sEEG lead localization. Raw SPECT images are coregistered to T1-weighted MRI sequence. SPECT deviation map is computed and anatomically colocalized with sEEG signals. Image courtesy of the Journal of Nuclear Medicine.
Schematic of triggered ictal SPECT and data processing. (A) Previously screened and selected sEEG bipolar contact is stimulated to trigger patient-typical seizure. Directly after seizure onset, confirmed through sEEG signals and semiology, systemic bolus of radiotracer (Tc-99m HMPAO) is administered. Planned SPECT is acquired within less than one hour. (B) Raw data processing from left to right (dataset from participant three as example). Postimplantation CT and preimplantation T1-weighted MRI are coregistered for sEEG lead localization. Raw SPECT images are coregistered to T1-weighted MRI sequence. SPECT deviation map is computed and anatomically colocalized with sEEG signals. Image courtesy of the Journal of Nuclear Medicine.
The ictal SPECT images subsequently contributed to characterizing periictal aphasia in all three participants, the group wrote. In two cases, ictal SPECT offered complementary information to sEEG and further revealed early involvement of brain areas that lacked electrode coverage, and in the third case, sEEG and ictal SPECT provided overlapping information.
“This is the first study establishing the feasibility of triggering ictal SPECT on demand with direct electric stimulation of the epileptic cortex,” the group wrote.
The authors noted that SPECT scanners and sEEG for recording and stimulation are broadly available at specialized epilepsy centers. Thus, novel data generated with the technique in larger cohorts could help refine resection planning and improve seizure and cognitive outcomes in epilepsy surgery, they suggested.
“Triggering of patient-typical seizures for on-demand ictal SPECT may broadly reinstate this often-abandoned imaging technique and help tailor resective epilepsy surgeries,” the group concluded.
A link to the full article can be found here.