A lexicon used to describe findings on molecular breast imaging (MBI) exams does a good job of predicting the malignancy of lesions, suggests a study published July 20 in the American Journal of Roentgenology.
A team led by Dr. Katie Hunt from the Mayo Clinic in Rochester, MN, found that terms -- or descriptors -- from the lexicon had a high positive predictive value (PPV) for predicting malignancy.
"This understanding of descriptors that favor benignity and malignancy can assist radiologists' interpretations and help improve the specificity of molecular breast imaging," Hunt and colleagues wrote.
MBI uses a small-field-of-view gamma camera to image radiotracer uptake within the breast, and it is used as a supplement to screening with standard digital mammography or to guide treatment. Previous research suggests that MBI has a supplemental cancer detection rate of eight to nine cancers per 1,000 women screened when used along with digital mammography.
Breast radiologists developed a lexicon in 2012 for MBI that mirrors the lexicon used for imaging descriptors in the BI-RADS atlas. This lexicon includes descriptors for mass versus nonmass radiotracer uptake, distribution of nonmass uptake, and lesion intensity.
But how accurate are the terms in the lexicon? Little data exists on the predictive value of the lexicon descriptors in determining whether breast lesions are benign or malignant, so Hunt et al investigated the issue. They noted that having knowledge of the PPV for a lexicon is a must for applying breast imaging modalities into clinical practice.
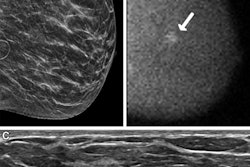
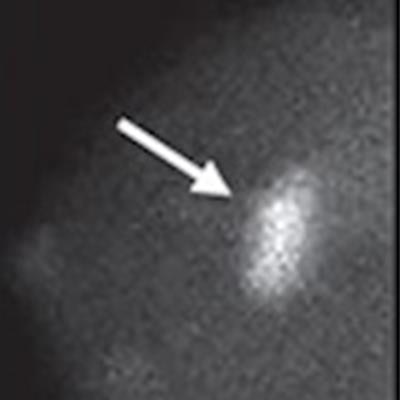
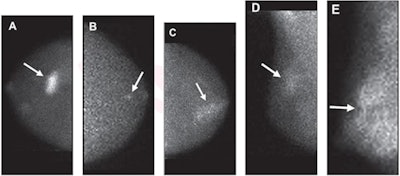 Molecular breast images show (A) mass (arrow) with marked intensity of uptake; (B) nonmass uptake (arrow) with focal distribution and mild intensity of uptake; (C) nonmass uptake (arrow) with segmental distribution and moderate intensity of uptake; (D) nonmass uptake (arrow) with regional distribution and mild intensity of uptake; and (E) nonmass uptake (arrow) with diffuse distribution and marked intensity of uptake. Image courtesy of the American Journal of Roentgenology.
Molecular breast images show (A) mass (arrow) with marked intensity of uptake; (B) nonmass uptake (arrow) with focal distribution and mild intensity of uptake; (C) nonmass uptake (arrow) with segmental distribution and moderate intensity of uptake; (D) nonmass uptake (arrow) with regional distribution and mild intensity of uptake; and (E) nonmass uptake (arrow) with diffuse distribution and marked intensity of uptake. Image courtesy of the American Journal of Roentgenology.They looked at retrospective data from 643 lesions in 509 patients, collected between 2005 and 2017. The lesions had BI-RADS analogous categories of 0, 3, 4, or 5. Out of the total, 479 lesions were found to be benign and the other 164 malignant. Also out of the total, 83 were categorized as masses while the remaining 560 had nonmass uptake.
| Accuracy of MBI lexicon descriptors for predicting malignancy | |
| Descriptor | Positive predictive value (PPV) |
| Type of lesion uptake | |
| Mass uptake | 73.5% |
| Nonmass uptake | 18.4% |
| Intensity of uptake | |
| Marked uptake | 64.8% |
| Moderate uptake | 22.4% |
| Mild uptake | 14% |
| BI-RADS rating of lesion | |
| Category 5 | 87% |
| Category 4 | 40.1% |
| Category 3 | 1.8% |
| Category 0 | 4.7% |
The researchers also found that the more MBI views that a finding was visible on, the higher the likelihood of malignancy: Lesions that were visible on four MBI views had a 45.4% likelihood of malignancy.
The study authors concluded that these findings highlight the importance of interpreting MBI for radiologists. They added that it's also important for radiologists to recognize the value of conventional diagnostic imaging in diagnosis and management of molecular breast imaging findings and to use conventional imaging before recommending follow-up or biopsy.
"In addition, as molecular breast imaging continues to be integrated into breast imaging practices, the findings could be used to inform the Committee on BI-RADS regarding the possible incorporation of the molecular breast imaging lexicon into the BI-RADS Atlas," they wrote.