Researchers in France say radiation doses in PET/MRI exams can be reduced significantly without compromising image quality in patients with neurological disorders, according to a study published September 12 in Scientific Reports.
A group at Sorbonne University in Paris simulated PET/MRI imaging with a 90% reduction in injected F-18 FDG radiotracer dose in patients with cognitive impairment. The images remained reliable for differentiating Alzheimer's disease and frontotemporal dementia, according to the findings.
"The ultralow-dose protocol offers a possibility of substantial reduction in ionizing radiation exposure," wrote medical physicist Marine Soret, PhD, and colleagues.
In the last five years, PET technology has improved significantly, with hybrid PET/MRI scanners offering increased axial field of views that result in higher sensitivity. For brain F-18 FDG-PET/MRI, reducing total PET acquisition time (and thus radiation exposure by F-18 FDG) is limited by MRI, however, which usually requires an image acquisition time of 20 minutes or more.
Thus, the researchers suggest that increasing PET acquisition time to match that of MRI allows the dose of F-18 FDG radiotracer to be decreased. In previous work, the group has shown that radiotracer activity can be reduced to 1 MBq/kg versus standard 2 MBq/kg without significantly degrading image quality. In this feasibility study, they aimed to reduce injected F-18 FDG activity by 10-fold.
The authors used a previously validated method to simulate a 0.2 MBq/kg dose of injected FDG. Essentially, they reconstructed a second set of images from data acquired during the first two minutes of the standard PET/MRI scan (Signa PET/MRI, GE Healthcare), with the scanner's parameters optimized by physicists to ensure a high signal-to-noise ratio.
The researchers then compared imaging from the simulated ultralow-dose PET/MRI protocol with imaging from the standard protocol in 50 patients with cognitive impairment. They compared visual analyses of the methods by three experienced physicians.
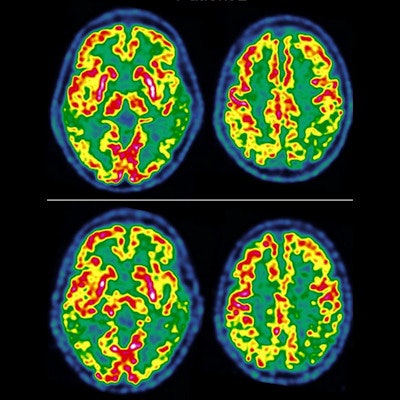
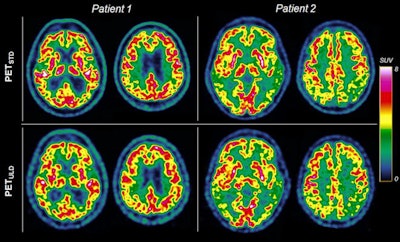 Transverse slices of two patients suspected of Alzheimer's disease with mild hypometabolism (patient 1) and severe hypometabolism (patient 2) with standard-dose (PET/STD, 2 MBq/kg) and ultralow-dose (PET/ULD, 0.2 MBq/kg) protocol. The transverse slices are extracted from the Advantage Workstation (AW server 3.2, GE Healthcare) used to carry out the interpretation. Image courtesy of Scientific Reports.
Transverse slices of two patients suspected of Alzheimer's disease with mild hypometabolism (patient 1) and severe hypometabolism (patient 2) with standard-dose (PET/STD, 2 MBq/kg) and ultralow-dose (PET/ULD, 0.2 MBq/kg) protocol. The transverse slices are extracted from the Advantage Workstation (AW server 3.2, GE Healthcare) used to carry out the interpretation. Image courtesy of Scientific Reports.The physician readers classified F-18 FDG PET patterns into seven categories: normal (N), nonevaluable (NE), Alzheimer's disease (AD), logopenic variant progressive primary aphasia (lvPPA), posterior cortical atrophy (PCA), semantic variant progressive primary aphasia (svPPA), and frontotemporal dementia (FTD).
Based on a consensus reading of images with standard F-18 FDG dose amount, exams were visually normal in 16 patients and suggestive of Alzheimer's disease in 15, svPPA in six, FTD in eight, and lvPPA or PCA in five.
According to the findings, intraoperator agreement between standard-dose FDG (2 MBq/kg) and ultralow-dose FDG (0.2 MBq/kg) for visually classifying patients into the seven categories was almost perfect in one rater and substantial in the other two (≥ 0.71) over the whole group.
In addition, group comparisons of radiotracer uptake between the 15 patients with Alzheimer's disease and eight patients with frontotemporal dementia on successive scans using both methods generated very similar results, the authors wrote. As expected, uptake ratios were significantly decreased in Alzheimer's disease compared with FTD in the parietal, precuneus, and lateral occipital cortices (p < 0.005).
The researchers concluded that performing 20-minute brain PET/MRI with F-18 FDG activity reduced to as low as 0.2 MBq/kg is feasible without compromising quantitative measurements.
"It does not change either imaging diagnosis in patients with clear regional anomalies," the researchers wrote of the protocol.
Ultimately, this was a feasibility study showing that an ultralow-dose protocol involving a 90% reduction of F-18 FDG injected activity did not significantly modify assessments of brain PET/MR images. This suggests that an activity as low as 0.2 MBq/kg may be sufficient for differentiating Alzheimer's disease from FTD, the group wrote.
Reducing the injected dose of F-18 FDG can significantly reduce radiopharmaceutical costs in a department performing a lot of FDG-PET scans, as well as improve radiation protection for young patients undergoing repeated scans, the authors wrote.
Based on these results, they recommend injecting 1-2 MBq/kg (70-140 MBq) for the early diagnosis of neurodegenerative disorders to guarantee a precise diagnosis and reserving the ultralow-dose protocol for subsequent scans.
"The ultralow-dose protocol offers a possibility of substantial reduction in ionizing radiation exposure, but should be reserved for the differential diagnosis or follow-up in patients with severe cognitive impairment or dementia," Soret and colleagues concluded.