Asian, Black, and Hispanic people participating in clinical trials for Alzheimer's disease have lower odds than white people for positive amyloid PET scans -- despite experiencing higher rates of the disease, according to a study published October 3 in JAMA Neurology.
U.S. researchers analyzed data from a large previous clinical trial evaluating the diagnostic use of amyloid PET scans in Medicare beneficiaries with mild cognitive impairment (MCI) or dementia. They found the proportion of amyloid-positive PET scans was greater among white participants compared with Asian, Black, and Hispanic participants.
The study suggests that clinical trials for new Alzheimer's disease drugs need to look beyond amyloid PET scans for reasons to include participants, the authors wrote.
"These results have important implications for the diagnosis, treatment, and prevention of [Alzheimer's disease] in groups that are at the highest risk of dementia," wrote corresponding author Dr. Consuelo Wilkins, a professor of medicine at Vanderbilt University Medical Center, and colleagues.
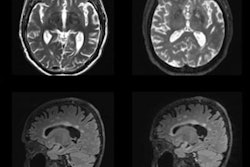
Amyloid PET scans are commonly used to identify eligible patients to participate in clinical trials for new Alzheimer's treatments and use various radiotracers to visualize deposits of amyloid plaque in areas known to be associated with the disease.
Although it is unclear exactly how amyloid plaque forms in the brain, research has shown that these amyloid deposits are involved in a cascade of events that lead to neurodegeneration and cognitive decline.
Research has also shown that social and structural risk factors, such as lived experiences of discrimination and racism, lack of economic opportunity, neighborhood disadvantages, and access to quality education may increase dementia risk for Black and Hispanic people, according to the group.
Given this backdrop, the researchers explored whether amyloid PET positivity rates differ across racial and ethnic groups with mild cognitive impairment or dementia. They performed a secondary analysis of data from the Evidence for Amyloid Scanning (IDEAS) trial, a study on the impact of amyloid PET on patient outcomes in Medicare beneficiaries.
The population in IDEAS consisted of Medicare beneficiaries 65 years and older diagnosed with MCI or dementia in whom the cause of cognitive impairment was uncertain after a comprehensive clinical evaluation. The study authors culled data on 17,107 participants who identified as Asian, Black, Hispanic, or white. They compared proportions of positive amyloid PET scans between matched racial and ethnic groups and then estimated their odds of having a positive scan.
According to the findings, the proportion of amyloid PET positive scans among Asian individuals and Hispanic individuals with MCI and dementia was 7% to 12% lower than matched white individuals and 4% lower among Black participants, although these differences were not statistically significant.
In addition, Asian, Black, and Hispanic participants had lower odds as expressed by hazard ratio (0.47-0.71) of amyloid PET positivity than white participants, the researchers stated.
"Despite disproportionately higher rates of dementia and clinical Alzheimer's disease among Black and Hispanic populations, we found lower odds of amyloid PET positivity among Black and Hispanic participants compared with white participants," they wrote.
The findings may reflect differences in the etiology of cognitive impairment, such as underlying vascular disease or social factors that impact health, the authors suggest. For instance, Black and Hispanic people experience higher rates of hypertension and diabetes, which are associated with nonamyloid brain changes linked to dementia, they wrote.
In addition, there is a current lack of inclusivity of diverse populations in clinical trials, and they noted that clinical trials for Biogen's recently approved Alzheimer's disease drug aducanumab included 10% Asian participants, 1% Black, and 3.4% Hispanic.
Ultimately, if diverse groups are not included in clinical trials for new treatments, there is a risk that novel treatment options will simply exacerbate existing racial and ethnic disparities in dementia care, the researchers noted.
To that end, the New IDEAS study was recently launched, which is focused on addressing these gaps by using multipronged recruitment and community engagement strategies to evaluate the clinical utility of amyloid PET in a more diverse cohort of patients, with a specific focus on recruiting Black and Hispanic Medicare beneficiaries, Wilkins and colleagues stated.
"Future research should include racially and ethnically diverse cohorts that reflect the burden of [Alzheimer's disease] in the population at large," they concluded.