Researchers have shed light on the Alzheimer’s disease “cascade hypothesis” – namely, the timing of biomarker progression that leads to neurodegeneration, according to a study published November 14 in Alzheimer’s and Dementia.
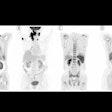
A group at the Mayo Clinic in Rochester, MN, studied associations between five Alzheimer’s disease biomarkers – two based on PET imaging and three blood-based biomarkers – and described their temporal evolution. The research is key to understanding the disease process, the group wrote.
“Associations of the timing of biomarker progression on the individual level indicate how closely two biomarkers are temporally linked and may inform disease mechanism,” noted lead author Petrice Cogswell, MD, PhD, and colleagues.
The cascade hypothesis in Alzheimer’s disease posits that beta amyloid accumulates in the brain years before a gradual spread of tau as clinical symptoms emerge. PET radiotracers that visualize both beta amyloid and tau protein have been developed that allow doctors to visualize this activity. Research has shown that circulating blood levels of tau protein (p-tau217, p-tau181) and glial fibrillary acidic protein (GFAP) can also be used to diagnose the disease, the researchers explained.
However, while previous studies have elucidated the relationships between plasma p-tau with beta-amyloid PET and tau PET, the timing of the development of these biomarkers is not well understood, the authors wrote. In particular, these associations have not been evaluated using statistical methods like “accelerated failure time” (ATF) modeling, a method that can show how associated variables affect the time it takes for an event to happen, they added.
Thus, the researchers employed an AFT model based on the development of beta-amyloid PET, tau PET, plasma p-tau217, p-tau181, and glial fibrillary acidic protein (GFAP) as endpoints.
The group included 1,408 participants with long-term data available from a Mayo Clinic Alzheimer’s disease study. Patients were all over 50 years old and had been diagnosed as cognitively unimpaired, mildly cognitively impaired, or with dementia.
According to the findings, individual timing of plasma p-tau progression was strongly associated with beta-amyloid PET and GFAP progression, with highlights including the following:
- Plasma p-tau progression was more strongly associated with beta-amyloid than tau PET.
- Progression on plasma p-tau was associated with beta-amyloid PET and GFAP progression.
- P-tau181 and p-tau217 become abnormal after beta-amyloid PET and before tau PET.
- GFAP became abnormal first, before plasma p-tau and beta-amyloid PET.
The researchers noted that beta-amyloid PET was estimated to become abnormal on average 13 years before tau PET, while plasma p-tau217 and p-tau181 were estimated to become abnormal approximately five to seven years after abnormal beta-amyloid PET and six to nine years before abnormal tau PET.
“In the population, GFAP became abnormal first, then beta-amyloid PET, plasma p-tau, and tau PET temporal meta-regions of interest when applying cut points based on young, cognitively unimpaired participants,” the group wrote.
Ultimately, the study strengthens the concept of the Alzheimer’s disease cascade hypothesis, with the timing of biomarker progression expected to inform precisely where in the disease process new therapeutic targets may be most effective, the authors suggested.
“Future studies will include evaluation of these temporal relationships using alternative plasma p-tau assays and a more demographically diverse sample,” the group concluded.
The full article is available here.