AI can effectively predict hospitalization for acute heart failure exacerbation in patients undergoing SPECT/CT myocardial perfusion imaging (MPI), according to a team of U.S. researchers.
Ultimately, the model could enable early interventions to prevent heart failure hospitalizations and lead to improved patient outcomes, noted lead author Attila Feher, MD, PhD, of Yale University in New Haven, CT, and colleagues at the University of California, Los Angeles.
“This study represents the first evidence, to our knowledge, demonstrating that integrating SPECT MPI into an AI-based risk assessment algorithm significantly improves the prediction of hospitalizations due to [heart failure],” the group wrote. The research was published March 28 in the Journal of Nuclear Medicine.
Heart failure is a major cause of morbidity and mortality in the United States and worldwide, with prevalence projected to increase by almost 50% from 2012 to 2030, the authors wrote. They noted that identifying patients who are at risk for heart failure exacerbation can open opportunities for prevention strategies.
AI has been previously used to predict potentially fatal events in patients with cardiovascular artery disease undergoing SPECT MPI, yet an AI model has yet to be developed that can predict heart failure exacerbations, they added.
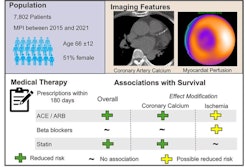
To that end, the researchers culled data from a registry of patients who underwent dedicated nuclear cardiology SPECT imaging using cadmium zinc telluride solid-state detector systems (Discovery NM 530c or Discovery NM/CT 570c, GE HealthCare) at two sites: Yale University and the University of Calgary.
The heart failure risk prediction model was developed using the Yale University cohort (n = 4,766) and was trained to make decisions based on standard clinical risk factors, SPECT imaging parameters, such as left ventricular ejection fraction (LVEF) measurements, and coronary artery calcium scores from CT scans. In this cohort, heart failure hospitalization occurred in 297 patients during a median follow-up of 1.9 years.
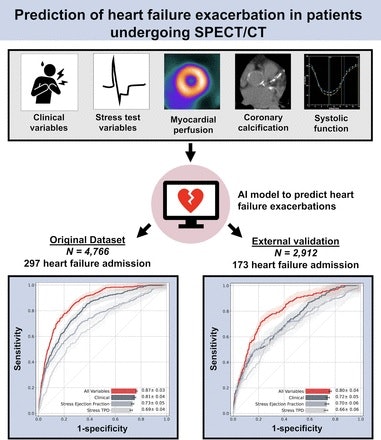 A visual abstract of the study by the authors. Image courtesy of the Journal of Nuclear Medicine.
A visual abstract of the study by the authors. Image courtesy of the Journal of Nuclear Medicine.
During testing, the model demonstrated an area under the receiver-operating-characteristic curve (AUC) of 87% for predicting heart failure admissions over a model that used stress LVEF (73%) to predict admissions or a model developed using only clinical parameters (81%).
To confirm these findings, the researchers tested the AI model in the cohort from the University of Calgary (n = 2,912), which included 173 patients hospitalized for heart failure during a median follow-up of 2.7 years. In this group, the model achieved an AUC of 80% for predicting admissions versus 70% for the model using stress LVEF and 72% for the clinical model.
“The results show that including results from SPECT/CT MPI, such as LVEF, myocardial perfusion, stress test parameters, and coronary calcifications, significantly improves the identification of individuals at the highest risk of [heart failure]-related hospitalization,” the group wrote.
The investigators noted that the study did not compare the AI model to estimates of heart failure hospitalizations based on expert physician opinions and also that the study used data from high-spatial-resolution systems compared to conventional SPECT systems.
Nonetheless, the research opens the door for studies with significant clinical implications, they wrote.
“Further studies are needed to evaluate whether therapeutic interventions guided by our AI predictions can effectively modify the risk of future heart failure hospitalizations in patients undergoing SPECT MPI,” the researchers concluded.
The full study is available here.