PET brain scans show persistent brain inflammation in patients with multiple sclerosis (MS), despite being treated with high-efficacy disease-modifying therapies, according to a recent study by researchers in Boston.
The finding suggests that PET imaging of translocator protein (TSPO) in the brain can serve as a biomarker for evaluating patients whose disease progresses despite treatment, noted lead author Tarun Singhal, MD, of Brigham and Women’s Hospital and colleagues.
“One of the perplexing challenges for clinicians treating patients with MS is after a certain amount of time [is that] patients continue to get worse while their MRIs don’t change,” Singhal said, in a news release from Brigham.
“Smoldering” inflammation is a term recently popularized to describe widespread innate immune activation present beyond focal inflammatory lesions in MS patients. This persistent inflammation increases atrophy of gray matter in the brain, yet is difficult to assess on MRI scans, the authors explained.
In a study published April 17 in Clinical Nuclear Medicine, the group at Brigham tested a new TSPO radiotracer they developed for visualizing such activity called F-18 PBR06. The tracer has a high affinity for binding to TSPO on microglial cells, known as the sentries of the brain’s immune system.
The researchers performed F-18 PBR06 PET scans on 22 patients with MS and eight healthy controls. They measured the “glial activity load” on the scans and compared results among patients with MS and healthy controls, as well as between individuals with MS on high-efficacy disease-modifying therapies (n = 13) and those on no or lower-efficacy treatments.
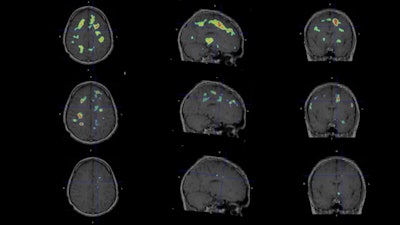 Individualized parametric z-score maps of the brain showing glial activity load in the brain, compared among individuals with secondary progressive MS (SPMS) (top row), relapsing-remitting MS (RRMS) (middle row), and a healthy control (HC) (bottom row) in transaxial, sagittal, and coronal sections. Image courtesy of Clinical Nuclear Medicine.
Individualized parametric z-score maps of the brain showing glial activity load in the brain, compared among individuals with secondary progressive MS (SPMS) (top row), relapsing-remitting MS (RRMS) (middle row), and a healthy control (HC) (bottom row) in transaxial, sagittal, and coronal sections. Image courtesy of Clinical Nuclear Medicine.
According to the analysis, glial activity on F-18 PBR06 PET scans was higher in patients with MS than healthy controls in cortical gray matter (+33%) and white matter (+48%). In addition, among MS patients treated with high-efficacy disease-modifying therapies, glial activity load was linked with increased cortical atrophy.
Moreover, the differences in MS patients on high-efficacy disease-modifying therapies were associated with worsening physical disability, and higher depression and fatigue scores, the authors added.
“This study tells us something new about the disease and may be giving us an important clue as to what is driving disease progression in patients,” noted Rohit Bakshi, MD, a co-author on the paper.
Ultimately, the study validates the use of F-18 PBR06 PET scans in these patients, with the tracer providing a longer half-life life than current tracers, according to the group. This allows extended imaging acquisition times to measure TSPO as a biomarker, the team wrote.
“This is a new approach that is potentially going to be very helpful for the field, for research, and hopefully for clinical use,” the researchers concluded.
The full article is available here.