A recently developed PET radiotracer identified sources of pain in patients with complex regional pain syndrome (CRPS) and led to effective treatments, according to a study presented June 10 at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) annual meeting.
Joe Baal, MD, a radiology resident at the University of California, San Francisco presented a whole-body PET/MRI study of a new pain-specific PET radiotracer named F-18 FTC-146 developed for identifying peripheral pain generators in patients with CRPS.
“The novel image findings obtained through the suggested PET/MRI approach have a positive potential impact on pain management strategies for CRPS patients, leading to enhanced outcomes and more efficacious pain treatments,” Baal said.
Complex regional pain syndrome (CRPS) is a chronic pain condition that affects millions of patients worldwide. It is a form of chronic pain that usually affects an arm or a leg and typically develops after an injury, surgery, stroke, or heart attack, Baal explained.
“CRPS can be so debilitating that these patients can be very depressed and sometimes it’s even called the ‘suicide disease’ because of the elevated suicidal risk these patients experience,” he said.
Currently, the underlying mechanism of CRPS is not well understood, and diagnosing it can be difficult due to its heterogeneous clinical presentation and the absence of specific tests that can identify what generates the pain, he noted.
To that end, Baal and colleagues developed F-18 FTC-146. In preclinical studies, the researchers established that the tracer binds to sigma-1 receptors (S1R) on neurons and glial cells involved in states of inflammation or pain.
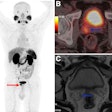
To investigate the usefulness of F-18 FTC-146, the researchers tested it in a prospective observational clinical trial in 15 patients (10 women, 5 men) with a clinical diagnosis of CRPS. The patients had an average duration of pain symptoms of five years and had previously undergone unsuccessful treatments. The participants underwent whole-body (head-to-toe) PET/MRI scans after tracer injection, with the findings subsequently discussed with the pain specialists who referred them to the trial.
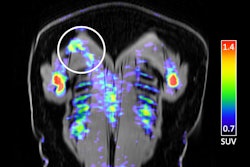
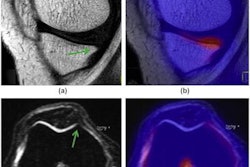
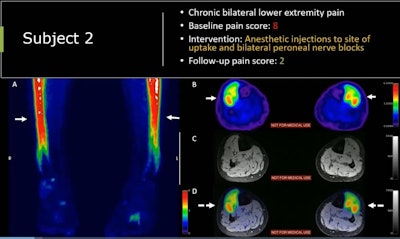 F-18 FTC-146 PET/MRI scan of a 21-year-old male soccer player who participated in the trial. The man had chronic bilateral lower expremity pain with a baseline pain score of 8 out of 10. Based on the finding, the patient underwent anesthetic injections and nerve blocks at the site of radiotracer uptake and reported a pain score of two on a follow-up visit.Image courtesy of Joe Baal, MD
F-18 FTC-146 PET/MRI scan of a 21-year-old male soccer player who participated in the trial. The man had chronic bilateral lower expremity pain with a baseline pain score of 8 out of 10. Based on the finding, the patient underwent anesthetic injections and nerve blocks at the site of radiotracer uptake and reported a pain score of two on a follow-up visit.Image courtesy of Joe Baal, MD
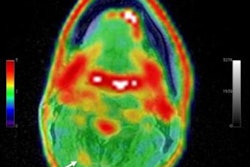
According to the results, unexpected findings and potential pain sources were observed on the F-18 FTC-146 PET/MRI scans in 12 out of the 15 patients (80%). Moreover, the findings prompted adjustments to pain management strategies for 61% (8 out of 13) of these individuals, Baal noted. Effective treatments included peripheral nerve blocks (n = 4), peripheral nerve decompression surgery (n = 2), and surgical removal of bone/soft tissue (n = 2).
“In conclusion, S1R-PET/MRI identified potential pain generators based on increased S1R density … larger studies are needed for validation and exploration of this agent in other pain syndromes,” he said.