Long axial field-of-view (LAFOV) PET/CT scanners offer shorter procedure times and avoid the need for sedation or general anesthesia when imaging young children with neuroblastoma, according to a recent pilot study.
A group at Copenhagen University Hospital in Denmark found that a new LAFOV PET/CT scanner identified a higher number of lesions in patients than standard SPECT/CT, as well as avoided the need for general anesthesia and sedation.
“[LAFOV PET/CT] shows promise for future staging and response assessment in children with neuroblastoma,” noted lead author Lise Borgwardt, MD, PhD. The study was published July 3 in the Journal of Nuclear Medicine.
Neuroblastoma is a cancer that develops from immature nerve cells found in several areas of the body. It is the most common extracranial solid tumor in children and more than 50% of patients present with metastases at diagnosis, with an overall survival rate of about 50%.
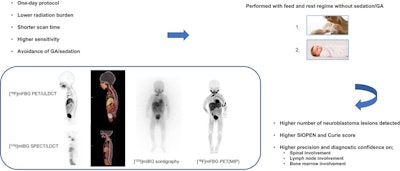
For decades, the standard approach for imaging the disease has been a two-day SPECT/CT protocol, with a 24-hour iodine-231 (I-231) meta-iodobenzylguanidine (MIBG) radiotracer tracer uptake period. In addition, sedation or general anesthesia is often used because of a lengthy scan time, often over two hours, the researchers noted.
Hence, in this study, the group initiated a prospective study to evaluate the feasibility of using a new LAFOV PET/CT scanner (Biograph Vision Quadra, Siemens Healthineers), which was launched in Europe in 2020 and approved in the U.S. in 2021.
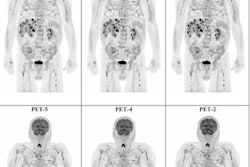
In total, 10 children with a median age of 1.6 years old (range, 0.1 to 7.9 years old) underwent both I-231 MIBG SPECT/CT and LAFOV PET/CT with a new PET radiotracer called F-18 MFBG. Five children were scanned at the time of diagnosis, two during treatment, two during off-therapy surveillance, and one at verified relapse.
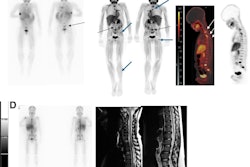
 A visual abstract of the study.Image courtesy of the Journal of Nuclear Medicine
A visual abstract of the study.Image courtesy of the Journal of Nuclear Medicine
According to the analysis, F-18 MFBG PET/CT scans showed a higher number of radiotracer-avid lesions in 80% of the cases and an equal number of lesions in 20% of the cases. In particular, intraspinal, retroperitoneal lymph node, and bone marrow involvement were diagnosed with much higher precision, the researchers noted.
In addition, none of the children had sedation or general anesthesia (GA) during the PET/CT procedure, whereas 80% had GA during SPECT/CT. A PET scan time of only 10 minutes was required to acquire clinically useful images, the group added.
“This pilot study demonstrates the feasibility of performing F-18 MFBG LAFOV PET/CT for imaging of neuroblastoma,” the authors wrote.
Ultimately, LAFOV PET/CT scanners are game-changing innovations at the threshold of clinical implementation, as they reduce the risks and logistical challenges associated with sedation by acquiring images faster, the group noted. These results in the first 10 children in a prospective study are preliminary and open the door for larger studies, they wrote.
“The impact on staging, treatment decision-making, treatment-response assessment, and off-therapy surveillance remains to be explored,” the researchers concluded.
The full study is available here.