AuntMinnie is pleased to present the final installment of a three-part series on Alzheimer's disease, based on research presented at the 2001 Society of Nuclear Medicine meeting in Toronto.
A decade ago, as researchers pondered a variety of pharmacologic approaches that might be used to delay, prevent, or even reverse the course of Alzheimer's disease (AD), the brain's cholinergic system emerged as a logical starting point.
AD's plaques and tangles were known to take a heavy toll on cholinergic function, a neurochemical balancing act in which acetylcholine works as a neurotransmitter and acetylcholinesterase breaks it down. In AD patients, the enzymes that synthesize acetylcholine can decline by as much as 90% in affected brain areas, while acetylcholinesterase activity remains largely intact. The resulting acetylcholine deficit has been directly correlated with cognitive decline.
Since 1993 the FDA has approved four drugs, known as acetylcholinesterase inhibitors, which increase available acetylcholine by slowing production of the enzyme that destroys it. First to hit the market was tacrine hydrochloride (Cognex), approved in 1993, followed by donepezil hydrochloride (Aricept) which joined the list in 1996.
Donepezil has several advantages over Cognex, including once-daily dosing, fewer side effects, and less-frequent monitoring of serum transaminase levels. A third drug, rivastigmine tartrate (Exelon), became available last year, and galantamine hydrobromide (Reminyl), a promising compound made from daffodil bulbs, was approved by the FDA in early 2001.
In large-scale studies, all of these drugs have moderately improved cognition, global function, and the ability to perform normal daily activities in patients with mild to moderate AD. However, patients with advanced AD have not responded to pharmacologic therapy, the only currently available treatment for the disease. The drugs' long-term benefits, even in patients with milder AD, remain unproven.
Following up on the latest research, groups presenting at this year's Society of Nuclear Medicine meeting in Toronto assessed cerebral blood flow with SPECT and digital autoradiography to evaluate the effectiveness of donepezil therapy in Alzheimer's patients.
One study measured rCBF in long-term donepezil users. Another sought to illuminate the drug's previously demonstrated effects (Journal of Neuropsychiatry and Clinical Neuroscience, Spring 2000;12(2):209-18) on relative cerebral blood flow (rCBF) in AD patients. The results suggest that donepezil therapy has its greatest effect on perfusion in the frontal cortices, and that its benefits may be only temporary.
99mTc-HMPAO follow-up in AD patients
First, a study by Dr. Guiliano Mariani, M. Carletto, P. Vitali, P. Erba and colleagues from the University of Genoa Medical School in Italy performed 99mTC-hexamethylpropylene amine oxime (99mTc-HMPAO) brain SPECT imaging to assess rCBF in patients undergoing donepezil treatment. The study found moderate improvements in perfusion and cognitive scores in more than half of the patients treated.
"We wanted to clarify the relationship between cerebral perfusion and the efficacy of treatment of AD with donepezil," Mariani said.
The group looked at 19 patients with probable AD based on National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer's Disease and Related Disorders Association (NINCDS-ADRDA) criteria.
"Our patient population ... all had mild to moderate Alzheimer's disease, with (Folstein Mini Mental State Examination) MMSE scores higher than 14," Mariani said.
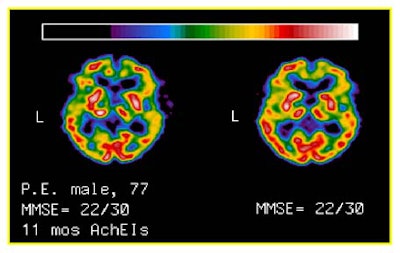
The patients, 15 women and 4 men aged 73.5 years (+/- 6.4 years) underwent clinical examination, neuropsychologic evaluation, and brain perfusion before therapy. The evaluations were repeated after approximately one year (10.6 months +/- 2.9 mo.) of continuous treatment with 5/mg/day of donepezil.
At baseline and follow-up, high-resolution brain SPECT was conducted using a dedicated gamma camera with an annular crystal (CeraSPECT, Digital Scintigraphics, Waltham, MA). SPECT data from both exams were compared with Statistical Parametric Mapping (SPM-99).
The software drew 30 regions of interest on the cortical ribbon of the frontal and parieto-temporal areas. Mean pixel counts of each ROI were normalized to those of the whole cerebellum, and statistical analysis was performed on all of the data.
The results were based on changes in MMSE scores following therapy, Mariani said. The patients were divided into 11 "responders," whose MMSE scores changed from 0.18 +/- 1.6 (range -1 to +2). Their ages were 78 +/- 6 years, and their baseline MMSE scores were 19.6 +/- 3.9.
There were 8 "nonresponders," whose MMSE scores changed -4.38 +/- 1.3 (range -1 to +2). Their ages were 73 +/- 6 years, and their baseline MMSE scores were 19.6 +/- 3.8.
 |
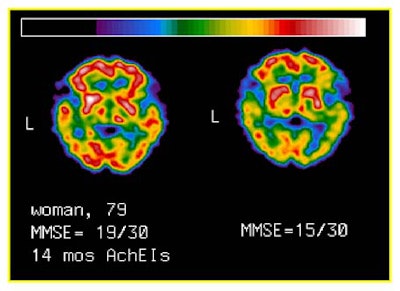 |
For example, there was a trend toward increased brain perfusion in responders, especially in the left parieto-temporal ROI. However, following (Bonferroni’s) adjustment for multiple comparisons, the increase did not reach statistical significance. No pattern of changes in brain perfusion was detected in nonresponders.
The only significant differences between responders and nonresponders were changes in MMSE score (<0.001) irrespective of age, sex distribution, and baseline MMSE, he said.
The responders showed a significant correlation between baseline MMSE scores and percentage rCBF changes in all ROIs, (R=0.47 to 0.7; P=0.05 to 0.01). The responders also showed significant correlation between the change in MMSE scores and rCBF percentage changes in all ROIs (R=0.61 to 0.8l; P=0.02 to 0.001), with the highest correlation in frontal ROIs.
"The message is that the patients with higher MMSE variations [following therapy] had milder [baseline] disease, at least in this particular case," Mariani said. "The second correlation is between the changes in MMSE scores and the change in cerebral perfusion" in the left parieto-temporal lobes. It may be that acetylcholinesterase inhibitor therapy is most effective in the better-preserved frontal areas of patients with mild AD, he said.
A statistical analysis of results based on multiple comparisons showed that increased perfusion in the left parieto-temporal area of responders is probably not significant "per se," Mariani said. However, he noted that other studies (e.g., Nuclear Medicine Communications, January 2000;21(1):37-41) have shown strong correlations between rCBF and cognitive function.
Donepezil ineffective with long-term use
In another presentation, researchers from the Kyoto Prefectural University of Medicine in Japan found that temporary perfusion increases associated with donepezil treatment did not persist in long-term therapy.
Dr. Yo Ushijima, along with colleagues C. Okuyama, T. Nakamura, T. Nishimura et al, examined the relationship between cerebral blood flow and MMSE scores using N-isopropyl-p-123Iiodoamphetamine (IMP) digital autoradiography, and found a strong correlation between cerebral blood flow and MMSE scores.
"Recent reports show that treatment with donepezil produce a clinical improvement of cognitive function compared to a placebo group," Ushijima said. "The objective of this study was to estimate changes in regional cerebral blood flow of patients with AD in short-term or long-term treatment with donepezil."
The study examined 59 patients with AD (21 men and 38 women, mean age 74 +/- 8 years), 13 of whom received donepezil therapy, Ushijima said. CBF measurements and MMSE exams were performed in 7 patients after three months of therapy (short-term therapy group) and in 7 patients following one to two years of donepezil treatment (long-term therapy group). Differential rCBF values in five patients were measured both short- and long-term.
"There were no significant differences in age or development of mental differences [between] these groups" before treatment, Ushijima said.
The researchers first defined regions of interest in the cerebral cortex (superior and inferior frontal cortices), motor cortex, parietal cortex, anterior and inferior frontal cortices, anterior and posterior temporal cortices, and hippocampus in each hemisphere.
"In the short-term group, changes in rCBF were noted in the frontal and parietal lobes and in the ... temporal lobe," Ushijima said. "The data provides support of evidence of such clinical changes as improvement in cognitive function after 12 weeks of treatment. The most significant changes were in the hippocampus."
The short-term therapy group showed significant increases in rCBF except in the hippocampus (mCBF 0.814 +/- 0.078). However, MMSE scores did not change.
"There were also changes in rCBF in the long-term therapy group. Post-treatment rCBF values were essentially the same as pre-treatment values, but [in] 2 [patients] were decreased in the parietal lobes. [rCBF] diminished slightly in one or two patients," Ushijima said.
MMSE scores were significantly lower (19.0 +/- 4.9) in the long-term patients, he said.
"Interestingly, rCBF values in the parietal and temporal lobes were decreased after the long-term medication ... but in the frontal lobe, the rCBF after long-term medication was still increased to a slight extent," Ushijima said.
Short-term increases in cortical rCBF values were not maintained throughout treatment, and cognitive symptoms also worsened over the course of therapy, Ushijima concluded.
In his annual discussion of SNM meeting highlights, Dr. Henry Wagner from Johns Hopkins University in Baltimore lauded the Kyoto study, and suggested that earlier knowledge of donepezil's poor long-term results could have saved a lot of money.
"This is the type of information that the pharmaceutical industry can use to decrease the enormous cost today of developing a drug," Wagner said. "About 80% of the drugs that go into phase III clinical trials fail to result in an approved drug. And many believe it's because we have not had sufficient objective evidence."
By Eric Barnes
AuntMinnie.com staff writer
October 18, 2001
Related Reading
Alzheimer's disease, Part II: Researchers tackle progression, prediction, October 2, 2001
Alzheimer's disease, Part I: PET yields surprising findings in hippocampus, September 7, 2001
PET predicts future cognitive decline, June 26, 2001
PET, SPECT differ in Alzheimer's imaging, June 25, 2001
Nycomed Amersham, Neurochem to collaborate on Alzheimer's agents, July 19, 2001
New Alzheimer's guidelines reflect recent "explosion of information," May 8, 2001
SPECT increases accuracy of Alzheimer's diagnosis, April 19, 2001
New PET radiotracer could replace FDG for detecting Alzheimer’s, March 26, 2001
PET and MRI race to detect early Alzheimer’s, January 22, 2001
Copyright © 2001 AuntMinnie.com