SAN DIEGO - Hybrid PET-CT is all the rage in medical imaging, but when is it appropriate to use this powerful but expensive technology? A radiologist from the first hybrid PET-CT site in the world addressed the question at this week’s Academy of Molecular Imaging meeting.
The first combination PET-CT system was developed in the mid-1990s under the leadership of David Townsend, Ph.D. at the University of Pittsburgh, who worked with PET firms Siemens Medical Solutions of Iselin, NJ, and CPS Innovations of Knoxville, TN. CPS is a joint venture between Siemens and CTI Molecular Imaging, also of Knoxville.
Pittsburgh installed the first prototype machine in 1998; the first system cleared by the Food and Drug Administration was installed in 2001, according to University of Pittsburgh radiologist Dr. Todd Blodgett.
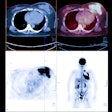
Hybrid scanners typically consist of PET and CT systems that have been arranged in a tandem configuration. The patient receives both the PET and CT scan in the same session, and the resulting data are fused into a single image that gives clinicians both anatomic and functional information.
The technique has proved particularly useful in oncology imaging, where CT’s anatomic component helps users localize the notoriously fuzzy PET images. At the same time, the FDG uptake produced by tumors can often help radiologists find small lesions that might be missed on CT.
Since installing their FDA-cleared scanner, the Pittsburgh group has scanned 1,700 patients. They have found that PET and CT images acquired in the same scan are more useful than PET and CT images taken separately. "There is a synergy that occurs when you have exact co-registration of the images," Blodgett said.
A number of factors weigh on the decision to perform PET-CT in lieu of separate PET or CT studies. These include scanner availability, the reason for the imaging request, and the patient’s recent anatomical imaging history. But probably the most important factor is the type of malignancy involved.
Head and neck malignancies represent one of the most promising areas for PET-CT, Blodgett said. The dense anatomical structures in the head can make it difficult to localize lesions on PET alone, while CT has trouble identifying lesions before they have caused anatomical or architectural distortion to tissue, he said.
PET-CT is useful for imaging thyroid cancer, particularly in cases of recurrence, he said. The best time for a scan is if a patient has had a thyroidectomy, rising thyroid globulin levels, and a negative CT or iodine-131 scan. In general, patients with an unknown primary tumor who present with neck masses are good candidates for PET-CT; the Pittsburgh group has done 20 such patients, and in 25%-30% of cases when they’ve had a negative CT scan the group has found a mucosal primary tumor.
Another area where PET-CT is more useful than PET alone is in colorectal cancer and abdominal/pelvic malignancies. PET alone is sometimes confounded by normal physiologic bowel uptake, while CT has difficulty differentiating recurrent cancer from normal postoperative tissue changes. The Pittsburgh group believes that anyone with suspected colorectal cancer is a good candidate for PET-CT.
PET-CT is appropriate for the staging and symptomatic restaging of lymphoma patients, Blodgett said. Again, PET can visualize lesions when they are small, in some cases as small as 6 mm, before they cause anatomic distortions to tissue. But if a patient is asymptomatic after treatment and has a negative PET-CT scan, follow-up surveillance will be done with either PET or CT independently in order to minimize radiation exposure, Blodgett said.
Cervical and ovarian cancer is another promising area for PET-CT, particularly in the realm of radiation-therapy planning. The technology can help identify the target volume of tumor and to assess response to radiation therapy, Blodgett said.
The jury is still out on the value of PET-CT for lung cancer applications, he said. There isn’t much normal physiological uptake in the chest, so PET alone is often sufficient. PET-CT can be useful for radiation-therapy planning, however, as well as biopsy localization, he said.
By Brian CaseyAuntMinnie.com staff writer
October 25, 2002
Related Reading
In-line PET-CT system improves cancer diagnosis, October 10, 2002
FDG-PET results keep colorectal cancer patients out of the OR, May 7, 2002
Swiss researchers optimize CT-PET scanning protocols, March 4, 2002
Copyright © 2002 AuntMinnie.com