TORONTO - Obesity is associated with abnormal coronary circulatory function and increases FDG uptake in large arteries, according to a pair of presentations at the Society of Nuclear Medicine (SNM) meeting this week.
Researchers from the David Geffen School of Medicine at the University of California, Los Angeles (UCLA) determined that increased body weight is associated with abnormal coronary circulatory function, which progresses from impairment in endothelium-related coronary vasomotion in overweight patients to impairment of the total vasodilator capacity in obese patients.
Meanwhile, in a study conducted at the Hospital of the University of Pennsylvania in Philadelphia, a research team demonstrated that large arteries in obese subjects are metabolically more active than those of over- and normal-weight patients.
Tipping the scales
Based on survey results from 1999 to 2002, the prevalence of overweight adults (a body mass index [BMI] value higher than 25 and less than 30 in the formula kg/m2) 20 years and older in the U.S. is 64%, while the percentage of adults in the same age range who are obese (BMI > 30) is 30%, according to the U.S. Centers for Disease Control and Prevention (CDC) National Center for Health Statistics.
In addition, the CDC notes that the prevalence of obesity has increased in the U.S. during the past 14 years. The 1991 Behavioral Risk Factor Surveillance System (BRFSS) survey found that four states had obesity prevalence rates of 15% to 19% percent, and no states had rates at or above 20%. By 2003, 15 states had obesity prevalence rates of 15% to 19%, 31 states had rates of 20% to 24%, and four states had rates higher than 25%.
The total economic cost to the U.S. for overweight and obesity is estimated at $117 billion, according to the Weight-control Information Network of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
The organization states that the direct cost of heart disease as a result of being overweight or obese, estimated at 17% of the total direct cost of heart disease independent of stroke, is $8.8 billion. Direct healthcare costs refer to preventive, diagnostic, and treatment services (for example, physician visits, medications, and hospital and nursing home care).
Myocardial blood flow
"The increasing prevalence of obesity in the U.S. is of considerable public health concern, and the mechanisms by which obesity initiates and accelerates vascular disease are still poorly understood," said Dr. Thomas Schindler in an SNM presentation. Schindler is from the department of molecular and medical pharmacology at UCLA's School of Medicine.
He presented the results of his research team's work on the relationship between obesity and coronary endothelial dysfunction as a precursor of coronary atherosclerosis, which may account for increased cardiovascular morbidity and mortality in obese individuals.
The group measured the myocardial blood flow (MBF) of 72 patients with a mean age of 37 years. There were 19 healthy (lean) patients with a BMI ≤ 25 who served as the control group, 21 overweight patients, and 32 obese patients, according to Schindler. Each patient was imaged with N-13 ammonia PET twice, once with a cold-pressor test (CPT), for mostly endothelium-dependent MBF, and once using dipyridamole-induced stress testing, for primarily endothelium-independent vasomotion.
The researchers found that MBF among the groups was similar at rest, but that MBF rates from rest to CPT were significantly attenuated in the overweight and obese groups than in the control group, and that the rates were significantly more reduced in the obese group than in the overweight group (p < 0.01).
"Hyperemic MBFs and, thus, the total vasodilator capacity were preserved in the overweight group as compared to normals but were significantly diminished in obese," Schindler said.
He also observed that progressive worsening is associated with an increase in plasma markers of the insulin-resistance syndrome, and that this might provide a mechanistic link between abnormal coronary vasomotion and at-risk cardiovascular outcomes.
"Quantitative PET imaging, with the assessment of the functional stage of the heart vessels, may indeed provide important information to stratify (or classify) the risk of an individual for future cardiovascular events," he said. PET imaging "may be a useful tool to monitor the effects of therapeutic interventions on impaired coronary vasomotor function to improve cardiovascular outcome in the long term."
Arterial avidity
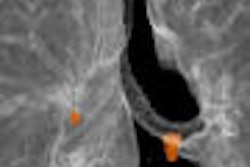
In an SNM poster presentation, researchers from the radiology department, division of nuclear medicine, at the Hospital of the University of Pennsylvania presented evidence that obesity correlates with increased FDG uptake in major arteries.
The group wrote that it examined 93 patients (43 male, 50 female; mean age 52.7 years) who underwent an FDG-PET scan for clinical purposes. The team examined two different age groups: 40 patients between 21-50 years old (18 male, 22 female; mean age 39.2 years) and 53 patients between 51-80 years of age (25 male, 28 female; mean age 62.9 years). Weight and height measurements were taken and BMI was calculated for each patient, then three subgroups of normal, overweight, and obese were established.
"In every patient, the degree of FDG uptake of the thoracic arteries (ascending, arch, and descending aorta) was measured using mean standardized uptake value (SUV)," the authors wrote.
The researchers reported that they found that increases in SUV in each region of the thoracic aorta correlated with the increments in BMI for both younger and older age groups. The results showed a statistically significant difference in all regions of the thoracic aorta between the normal-weight and obese patients (p < 0.05), as well as among the normal, overweight, and obese subgroups (p < 0.05).
Interestingly, the researchers determined that there was no statistical difference for mean SUVs between the normal and overweight groups of the 21-50 year olds in the ascending and the arch of aorta. And, they discovered that in the 51-80 year olds there was no statistically significant difference in SUVs of the overweight and obese groups for all regions of thoracic aorta.
"FDG uptake in large arteries as a marker for atherosclerosis may play a role in detecting effects of weight loss and other interventions in this population," they wrote.
By Jonathan S. Batchelor
AuntMinnie.com staff writer
June 22, 2005
Related Reading
Obese breast cancer patients may get subpar chemo, June 14, 2005
Voluntary weight reduction tied to bone loss in older men, April 22, 2005
Waist circumference better than BMI at predicting cardiac risk, February 23, 2005
Obesity in women linked with brain tissue loss, December 2, 2004
Obese women less likely to survive breast cancer, even after treatment, October 6, 2004
Copyright © 2005 AuntMinnie.com