PET and PET/CT have demonstrated superiority in staging most cancers, depending on the radiopharmaceutical tracer used in the imaging study. The technology has also proved its strength in myocardial perfusion exams. The next frontier for the modality may be determining the efficacy of drug therapies for oncology patients, according to multidisciplinary research presented last month at the 2006 Academy of Molecular Imaging (AMI) scientific meeting in Orlando, FL.
"If you look at the biodistribution of radioactivity following C-11 (carbon-11) topotecan injection with PET, you may be able to predict the therapeutic response," said Raymond Muzic, Ph.D. "More specifically, if no activity localizes in the tumor, then you might expect that this person would not respond to the topotecan therapy."
Muzic, an associate professor from the department of radiology at the Case Western Reserve School of Medicine in Cleveland, presented the results of a prospective study conducted by researchers at his institution, the U.S. Food and Drug Administration, the National Cancer Institute, and 3D Imaging of Cleveland. The project was a multidisciplinary study requiring the expertise of oncologists, chemists, nuclear medicine physicians, and others, he said.
"Topotecan is used as a second-line treatment for ovarian and small cell lung cancer," Muzic said. "According to the literature, 15% to 35% of people respond to topotecan. But I think this really overestimates what's really seen in clinical practice."
Muzic and his team set out to develop a method to predict if patients could benefit from topotecan therapy. If it was determined that they could not, oncologists could move on to another therapy that might prove more beneficial.
"This could potentially spare 65% to 85%, or maybe even a higher percentage, of these patients from getting topotecan," he said. "It also enables oncologists to expediently consider alternative therapy."
The team selected six female patients, five with ovarian cancer and one with small cell lung cancer with a mean age of 56, to participate in the study. All patients had been prescribed topotecan therapy by their oncologists; had a life expectancy of greater than 12 weeks; had measurable disease in a prior CT, MRI, or PET; and had a CT scan within four weeks of the study.
The researchers then labeled topotecan with carbon-11. This was accomplished through joint work begun by the FDA and concluded by 3D Imaging, according to Muzic. The FDA scientists knocked off the methyl group from topotecan and shipped the product to the researchers. The Cleveland team took the product, reacted it with carbon-11 methyl iodide, and put the radioactive methyl group back onto the topotecan.
"The result is topotecan," Muzic said. "It's not topotecan with some other group hanging off of it; it's actually the chemical."
They then established the radiation dosimetry and biodistribution of the radiopharmaceutical. Because this was the first use of the product on humans, the group erred on the side of caution, Muzic emphasized. They made the assumption that the injection amount would all go to one organ in the body, then calculated dose limits for that organ. They then repeated that process for all organs in the body and came up with dose limits that would allow them to stay within regulatory limits for safety, Muzic said.
"On that basis we came up with a somewhat low injected dose of 140 MBq," he said.
The team then conducted CT and PET imaging of the patients. This data allowed them to determine regions of interest, time-activity curves, and calculate resonance times. The resonance times permitted further refinements of the radiation dosimetry.
"We now had real data to estimate the radiation dosimetry," Muzic said. "We know the radiation dose to the various organs wasn't quite as large as our worst case calculations."
On the basis of the data, the team was allowed to increase the injected dose of the topotecan, he noted.
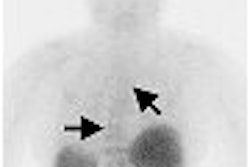
The researchers then set out to predict the efficacy of topotecan therapy. They administered subtherapeutic quantities of C-11 topotecan to the study group and imaged its biodistribution with PET. On a separate day, F-18 FDG biodistribution was also imaged with PET, to identify metabolically active tumors. The images were then reviewed and compared to see if C-11 uptake took place in areas of F-18 FDG tumor activity.
In all patients, the uptake of C-11 activity did not correlate with FDG uptake. On this basis, the researchers predicted that topotecan therapy would be ineffective, Muzic said. Clinical follow-up confirmed the group's prediction with a mean of 13 weeks to progression (±11 weeks) for the patients after they underwent topotecan therapy.
"Of course, the limitation to this is that we would have liked to have seen somebody who had actually had a response (to C-11 topotecan), but we just haven't had a patient like that yet," Muzic said. "We're going to continue these studies to hopefully find a patient like that and in parallel start working in animal models."
Although the patient cohort was small, and to date has succeeded in establishing a negative predictive value for topotecan therapy, the protocol shows promise for being extended to other drug therapies. In theory, this technique could determine within one day the efficacy of a particular therapeutic regimen, which may someday prove to be invaluable to the practice of oncology.
"One thing I want to point out is that this technique for topotecan could be applied for other drugs as well," Muzic said. "The trickiest thing would be getting the chemistry down -- making sure that you could provide the compound."
By Jonathan S. Batchelor
AuntMinnie.com staff writer
April 21, 2006
Related Reading
Rubidium-based PET may finally get its due, February 23, 2006
Therapeutic radiopharmaceutical market poised for takeoff, February 21, 2006
FDA issues draft CGMP for PET radiopharmaceuticals, September 26, 2005
Changing market for PET brings challenges and opportunities, September 30, 2004
Nuclear medicine group finds making FDG in-house to be feasible and affordable, December 3, 2003
Copyright © 2006 AuntMinnie.com