The pairing of external-beam radiation therapy (EBRT) followed by brachytherapy has shown strong results in long-term biochemical relapse-free survival (BRFS) rates in prostate cancer patients. A prospective cohort study conducted between January 1987 and December 1993 in Seattle has demonstrated that low- and intermediate-risk patients experience high disease-free survival rates with this treatment.
"Today's improved patient selection and improved implant quality has resulted in multiple brachytherapy reports demonstrating five- to 10-year BRFS rates are equivalent to the best published prostatectomy and three-dimensional conformal radiation therapy results," the study authors wrote in this month's International Journal of Radiation Oncology, Biology, Physics (January 2007, Vol. 67:1, pp. 57-64).
A total of 232 patients who presented with clinically localized prostate cancer during the six-year period were consecutively treated with EBRT and either iodine-125 (I-125) or palladium-103 (Pd-103) brachytherapy.
"Seven patients did not meet the initial cohort criteria for inclusion because of androgen ablation therapy for downsizing purposes and one patient had inadequate follow-up, reducing the analytic cohort to 223," the authors noted.
Each of the patients in the study was evaluated with a physical exam, digital rectal exam (DRE), and prostate-specific antigen (PSA) test every three to six months in the first two years after seed implant; then every six months for the next three years, and once every year thereafter. Tumor stage was assigned by DRE results, according to the scientists.
"Postimplant quality assurance was by the use of orthogonal films between 1987 and 1991," the authors wrote. "In 1992 postimplant CT scan dosimetry was performed."
Approximately four weeks prior to the ultrasound-guided permanent interstitial implant of either I-125 or Pd-103 seeds, the patients received 45 Gy of neoadjuvant EBRT.
"Patients did not undergo lymph node dissections or androgen ablation therapy," the authors wrote. "Any patient receiving androgen ablation therapy at any time after treatment, for any reason (e.g., benign PSA bounce), for any duration, is counted as a biochemical failure."
The 15-year BRFS for the entire group was 74%, the researchers reported. The low-risk group (those with a tumor stage of T2c or lower, an initial PSA of 10.0 ng/mL or less, and a Gleason summary score of 2-6) demonstrated a BRFS of 88%. The intermediate-risk group (those presenting with one of the following: T2b or higher, an initial PSA greater than 10.0 ng/mL, and a Gleason score higher than 6) had a BRFS of 80%, while the high-risk group (two or more of the following: T2b or higher, an initial PSA greater than 10.0 ng/mL, and a Gleason score higher than 6) showed a BRFS of 53%.
The researchers noted that since the inception of the study they have altered their treatment protocol for low-risk patients.
"The low-risk patients in this report received combination EBRT plus brachytherapy because of the authors' perception that they may be higher risk for relapse from a high number of positive biopsies and the virtual total lack of outcomes data with ultrasound-guided brachytherapy at the time we treated those patients," they wrote. "Currently, we rarely use combination brachytherapy plus EBRT in low-risk patients."
Most striking about the results of the study is that its 15-year BRFS rate of 74% is higher than the 66% BRFS rate reported for radical retropubic prostatectomy (RRP) in a recent study conducted at Johns Hopkins Hospital in Baltimore, as well as the 68% BRFS reported for RRP by researchers at Washington University in St. Louis (Journal of Urology, February 2003, Vol. 169:2, pp. 517-523; September 2004, Vol. 172:3, pp. 910-914).
The authors observed that, although the results of their study show strong support for EBRT and brachytherapy in treating prostate cancer, the patients represent an older era of treatment and less sophisticated technique.
"We expect improved BRFS outcomes in modern patients treated with modern brachytherapy equipment and techniques," they wrote.
By Jonathan S. Batchelor
AuntMinnie.com staff writer
January 25, 2007
Related Reading
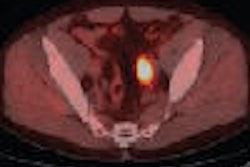
New tracer shows promise for PET/CT prostate imaging, January 18, 2007
Prostate cancer costs vary significantly by treatment type, January 10, 2007
Men with localized prostate cancer benefit from definitive treatment, December 18, 2006
Bone scans not needed in men with low PSA after localized prostate cancer therapy, July 28, 2006
SPECT/CT pilots prostate brachytherapy in community setting, August 15, 2005
Copyright © 2007 AuntMinnie.com