A British study has found that FDG-PET/CT is worthwhile for assessing patients with occult head and neck primary tumors, but false positives remain "a shortcoming of the technique," and the hybrid technology cannot replace examination under anesthesia (EUA) and biopsies.
The report comes from the Paul Strickland Scanner Centre in Northwood, U.K., which analyzed the accuracy of FDG-PET/CT for detecting primary lesions in 78 patients (63 males, 15 females) with squamous cell and undifferentiated cancer neck nodes. FDG-PET/CT was utilized when conventional assessment failed to identify a primary cancer site. All the patients in the study were scanned at the center from March 2004 to January 2006. The results were presented at the 2007 RSNA meeting in Chicago.
"With head and neck occult primary cancers, treatment planning is very important because localizing the primary site can markedly alter the treatment plan," said Dr. Wai Lup Wong, one of the center's researchers. "In the United Kingdom, standard practice is to radiate the whole head and neck, including the site likely to harbor a primary site and nodule disease. By identifying the primary site, it will allow for more direct treatment, with a high dose to the primary cancer and lower dose to surrounding normal tissue."
Cancer confirmation
According to the study results, FDG-PET/CT identified the primary site of cancer in 30 of 78 patients. The findings were confirmed histologically, with 14 of the 30 sites at the base of the tongue and 14 primary cancers detected at the pharyngeal palatine tonsils. Sixteen of the 78 patients had "suspicious" FDG uptake in the PET/CT scan, which could not be confirmed subsequently at biopsy. Of those, 12 were at the pharyngeal palatine tonsils, with the other four at the base of the tongue.
The study also found FDG-PET/CT had a sensitivity of 100%, specificity of 64%, positive predictive value of 65%, and negative predictive value of 100%. Fifteen false-positive results were attributed to FDG uptake in the base of the tongue and palatine tonsils.
Twenty patients did not have EUA and biopsies prior to FDG-PET/CT scans. In those cases, FDG-PET/CT increased the yield of primary tumor detection in 14 of the 20 cases (70%). In the 59 patients who had EUA and biopsies, FDG-PET/CT increased the yield of primary tumor detection in 16 cases (28%).
 |
| FDG-PET/CT clinical images show a tonsillar cancer (above), a positive neck node, and lateral node (below). Images courtesy of Paul Strickland Scanner Centre. |
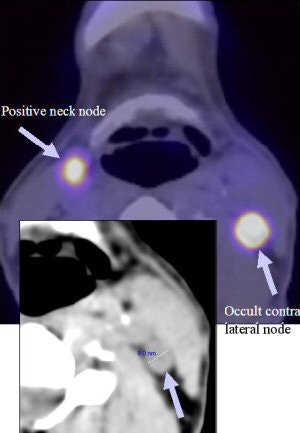 |
FDG-PET/CT also was able to detect unexpected sites of disease in six patients, who had uptake in contralateral neck nodes. In one patient, the discovery was confirmed by neck dissection, and by disease progression in another.
In four patients, the researchers were unable to confirm the FDG-PET/CT findings. "Two patients were treated with surgery to the primary site and radical neck dissection on the side of the primary site followed by chemoradiotherapy," Wong said. "One had a radical neck dissection on the side of clinical disease followed by chemoradiotherapy, and one other patient had palliative radiotherapy."
Clinical implications
The study also sought to determine FDG-PET/CT's value for patients who had tonsillectomies as part of their cancer evaluations. Researchers found that FDG-PET/CT should be considered in patients who had a tonsillectomy, because this group can yield occult primary cancers.
In the 28 patients who had EUA and tonsillectomy, FDG-PET/CT identified primary cancers in six cases. Four cancers were found in 16 patients who had unilateral tonsillectomies, and two cancers were discovered in 14 patients with bilateral tonsillectomies.
"Some clinical colleagues suggest that if patients have tonsillectomies, FDG-PET/CT is of limited value in showing occult primary lesions," Wong said. "I think our results show that FDG-PET/CT can be of value in identifying occult primary cancers, even in patients with tonsillectomies."
False positives
The main clinical implication from the British study confirms previous research that FDG-PET/CT is valuable for assessing patients with occult head and neck primary lesions, and the technology will detect unexpected primary cancers.
However, even with the promising results for FDG-PET/CT, the researchers noted that false positives remain a problem. "This occurs with normal lymph node tissue in the postnasal space and in the tonsils at the base of the tongue where they take up FDG. This area often harbors an occult primary cancer," Wong said. "Maybe a refinement in analyzing FDG update, in particular in the tonsils where occult primaries are probably the most common, can reduce the number of false-positive results in the form of SUVs."
Unexpected primary cancers in 10 of the 28 patients who had EUA and speculative biopsies, but no tonsillectomy, showed a false positive in four of 28 patients; there were no false-negative results.
This analysis is in contrast to a previous study by the same researchers with a similar group of patients, in which FDG-PET detected occult primary cancers in five of 17 patients. False positives were a factor with two patients and false negatives in three patients (Clinical Oncology, December 2003, Vol. 15:3, pp. 461-466).
"These comparative results suggest that PET/CT, in our hands at least, improves the detection rate of occult primary cancers, but does not lead to a reduction in the false-positive results," Wong said. "In our study, one false positive was due to glossitis and, in the other patients, FDG uptake was due to physiological uptake in lymphoid tissue."
Follow-up research
As for the next round of research, Wong suggests a prospective study to determine whether FDG-PET/CT can replace CT and MRI in assessing patients with occult primary cancers.
"The ultimate role of FDG-PET/CT remains unchanged. As with FDG-PET, it is to focus EUA on areas most likely to yield positive histology," he added. "The head and neck surgeon can use PET/CT to obtain a larger sample from suspicious areas, thereby increasing the diagnostic yield compared with speculative biopsies. Therefore, we can use FDG-PET/CT after full clinical assessment, if examination by flexible fiberoptic nasoendoscopy and MR or CT fails to show a primary."
By Wayne Forrest
AuntMinnie.com staff writer
January 31, 2008
Related Reading
SUVs need adjusting for high-resolution PET/CT, January 31, 2008
PET/CT shows its worth in cervical carcinoma, January 18, 2008
NOPR releases preliminary results of PET treatment strategies, January 11, 2008
SUV on FDG-PET can predict cervical cancer prognosis, September 19, 2007
ROI can influence quantitative FDG-PET study results, September 11, 2007
Copyright © 2008 AuntMinnie.com