CHICAGO - Researchers from Johns Hopkins University in Baltimore found that cardiac stress MRI not only outperforms SPECT for detecting acute myocardial infarction (MI) in patients presenting to the emergency room with chest pain, it reveals important information about the cause of the pain, even when symptoms are unrelated to coronary artery disease.
Triage of emergency room (ER) patients with chest pain is a common and expensive challenge for hospitals. Physicians must detect myocardial ischemia in the emergency room quickly and accurately, said Johns Hopkins radiologist Dr. Jens Vogel-Claussen in a presentation on Sunday. While electrocardiogram (ECG) and cardiac enzymes are the first-line tests to rule out acute myocardial infarction, there are many patients with negative enzymes and negative ECG results who remain at risk of MI, he said.
CT is becoming an option for evaluation of coronary artery disease in these patients, but myocardial SPECT perfusion imaging remains the primary modality for ruling out MI in these patients at Johns Hopkins, Vogel-Claussen said. Although SPECT benefits from a high negative predictive value, it is also known to miss small myocardial scars, and it suffers from attenuation problems. For this reason, the facility adds stress MRI to rule out large vessel disease owing to its high negative predictive value and sensitivity nearing 90% when delayed contrast enhancement is used, he said. For this study, the researchers compared SPECT to MRI to see how MRI might perform alone.
The study aimed to "assess the frequency of ischemic and nonischemic causes of chest pain using a comprehensive cardiac MR exam including adenosine stress perfusion imaging in emergency room patients compared to standard-of-care SPECT nuclear imaging," Vogel-Claussen stated.
The study evaluated 31 patients (mean age 55.2 years ± 12.6), all with negative cardiac enzymes who presented to the ER with chest pain and a referral for a technetium-99 nuclear stress test (SPECT, treadmill, dobutamine and adenosine stress).
"Cardiac SPECT was done within 24 hours of chest pain [onset] and MRI was done within three hours of SPECT, so it was really possible to do it within the emergency room setting," Vogel-Claussen said.
The MRI protocol included steady-state free precession (SSFP) cine imaging, T2-weighted TSE imaging, adenosine stress and rest perfusion imaging, and delayed enhancement MR imaging on a 1.5-tesla scanner (Siemens Healthcare, Malvern, PA). The high resolution SSFP stress perfusion sequence consisted of TR 2.4 msec/TE 1.0 msec, flip angle 50° 192 x 115 matrix). Gadopentetate dimeglumine (Magnevist, Bayer HealthCare Pharmaceuticals, Wayne, NJ) was injected at 5 cc/sec for the rest and stress perfusion MR images (0.05 mmol/kg). For the stress imaging sequence, 140 mcg/kg/min adenosine was administered intravenously.
"We did four categories of evaluation for stress imaging: one was reversible perfusion defect, the second was fixed perfusion defect, the third was diffuse subendocardial hypoperfusion with adenosine stress for small vessel disease, and the fourth was nonischemic cardiac findings," he said.
Four patients were excluded for claustrophobia in the MRI scanner, Vogel-Claussen said. Results in the remaining 27 patients showed moderately good agreement between SPECT and MRI for the presence or absence of reversible ischemia (24/27, 89%). Five patients (19%) had transient ischemia on MRI, which was confirmed on conventional angiography or coronary CT angiography showing a stenosis of 50% or greater. Only two (7%) of these cases showed transient ischemia on SPECT, he said.
In all, the cases included 10 normal patients, eight with small vessel disease, six with large vessel disease, and five with nonischemic cardiac findings, Vogel-Claussen said. The 10 normal cases at MRI were all normal on SPECT, but none of the eight small vessel disease cases or the five cases of nonischemic findings were detected on SPECT, he said.
Eight of the 27 patients (30%) had findings on MRI that could explain their chest pain other than proximal coronary artery disease. These included three cases of stress-induced diffuse subendocardial decreased perfusion (diabetes in two patients, cocaine use in one), pulmonary hypertension in two patients, one patient with previous mitral valve surgery, one with aortic insufficiency, and one with hypertrophic obstructive cardiomyopathy.
Among the six cases of large vessel disease there were five cases of reversible ischemia at MRI (two seen at SPECT); four of these cases also had fixed perfusion defects (three seen at SPECT). Of the three of reversible ischemia not detected by SPECT, two did not reach the target heart rate and one had triple vessel disease. Three cases also resulted from prior coronary artery bypass grafting and were therefore not clinically relevant.
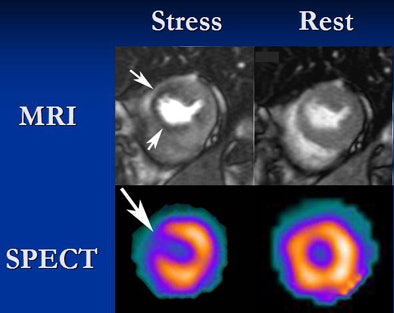 |
| In a patient with a fixed perfusion defect, MRI shows thickening in the LAD territory and hypoperfusion at stress which persists at rest, and scarring at delayed enhancement MRI (top). There is excellent correlation with SPECT images (bottom). All images courtesy of Dr. Jens Vogel-Claussen. |
Among the study's limitations, only patients with reversible ischemia on MRI underwent coronary angiography, and different methods were used to perform SPECT, he said.
"Adenosine-induced diffuse subendocardial hypoperfusion is common in the ED population with chest pain and negative enzymes," Vogel-Claussen said. "This is not detected with SPECT and may represent microvascular dysfunction. So what's the treatment? Why do we care? Maybe we should be more aggressive about this -- maybe we will find that these patients present more often to the emergency room than normal patients."
Cardiac stress MRI can pinpoint ischemic and nonischemic causes of chest pain in the ER, he concluded. MRI can improve the management of these patients, he said. In addition, coronary artery bypass graft patients may benefit more from high-specificity dobutamine stress testing.
Asked about the high rate (13%) of claustrophobia, Vogel-Claussen said that patients in the ED for chest pain tend to be worried and under a lot of stress. A moderator asked if it were really feasible to perform the complex protocol in an emergency room environment.
"I come from Johns Hopkins, but all cases were done at Bayview Medical Center, which is a teaching hospital," Vogel-Claussen said. "The techs had only a very limited knowledge of cardiac MR imaging at their hospital ... so I explained everything to them and built [the program] myself." While training takes a little extra effort at the outset, the results make it clear that the one-hour exam can definitely be done both in the ED and in a community setting, he said.
By Eric Barnes
AuntMinnie.com staff writer
November 30, 2008
Related Reading
Adenosine stress DECT equivalent to SPECT, MRI, November 21, 2008
MRI evaluation of chest pain cuts acute coronary syndrome, August 15, 2008
MR-IMPACT trial: CMR equivalent to SPECT for stenosis detection, February 18, 2008
Dipyridamole stress cardiovascular MRI predicts CAD outcomes, October 11, 2007
Cardiac MR measures predict pulmonary hypertension, April 9, 2007
Copyright © 2008 AuntMinnie.com