F-18 fluoroethylcholine (FEC) with PET/CT is showing early promise for radiation treatment planning of recurrent and primary prostate cancer, with greater doses of radiation delivered to PET/CT-positive lymph nodes, according to a study published online May 1 in Radiation Oncology.
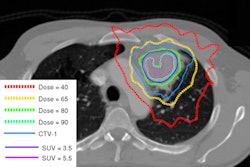
The study from Radiologische Allianz Hamburg noted that total radiation doses to lymph nodes are generally limited to less than 60 Gy. In this study, researchers found that total doses for metastatic lymph nodes of as much as 66.6 Gy applied with intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) "are safe and well tolerated," thus heightening the potential therapeutic benefit to patients.
Currently, there is no consensus on irradiation treatment volumes for intermediate- to high-risk primary cancers or recurrent disease, wrote lead study author Dr. Florian Wuerschmidt and colleagues. Conventional imaging modalities such as CT, MRI, and transrectal ultrasound are considered "suboptimal" for treatment decisions.
The researchers theorized that FEC-PET/CT combined with IMRT and IGRT "might offer the opportunity of dose escalation to selected sites while avoiding unnecessary irradiation of healthy tissues."
A total of 26 patients with a mean age of 65 years (seven patients with primary prostate cancer and 19 patients with recurrent prostate cancer) received FEC-PET/CT for staging and radiation therapy treatment planning. The majority of recurrent prostate cancer patients were considered intermediate to high risk.
Previous therapy for recurrent cancer was radical prostatectomy with or without lymphadenectomy in 16 of the 19 cases. Two patients had transurethral resection with seed implantation or antihormonal therapy, while one patient had radiotherapy of the prostate gland only. Among the seven primary cancer cases, five patients were treated with neoadjuvant and/or adjuvant antihormonal therapy.
Scans were performed on a hybrid PET/CT system (Biograph 16, Siemens Healthcare). All patients fasted for at least four hours before 3D FEC-PET imaging at three minutes per bed position. After FEC injection (350-500 MBq, 5 MBq/kg), a dual-time PET/CT scan was conducted from skull base to the upper thigh. Image acquisition included the pelvis and lower abdomen, starting two minutes after tracer injection.
Standardized uptake values (SUVs) were also calculated as SUVmax values.
Radiation treatment
Patients were treated five times weekly with a median radiation dose of 75.6 Gy (range, 72-75.6 Gy) for primary cancer and 66.6 Gy (range, 55.8-75.6 Gy) for recurrent disease.
The researchers determined clinical outcome from regular follow-up visits six to eight weeks after completion of radiotherapy and every six to 12 months thereafter, and/or with a questionnaire or telephone consultations with urologists assigned with the primary care of the patients. The median follow-up time was 28 months.
Final results showed that FEC-PET/CT studies were positive in 24 of 26 cases (92%). One patient with primary cancer had bone metastases and bladder infiltration, while one other patient experienced FEC uptake in the prostate gland and pelvic lymph nodes.
The two patients with negative PET/CT scans had prostate-specific antigen (PSA) values less than 1 ng/mL at the time of the scans. Overall, the median PSA at the time of PET/CT was 10.4 ng/mL (range, 0.2-115 ng/mL) for primary cancer and 1.9 ng/mL (range, 0.42-65 ng/mL) for recurrent cancer.
The study also found a mean SUVmax among primary cancer cases of 5.97 (range, 3.8-8.2) in the prostate gland and 3.2 in pelvic lymph nodes. Patients with recurrent cancer had a mean SUVmax of 4.38 (range, 1.6-15.3).
FEC uptake
FEC uptake was found in recurrent tumors in the prostatic bed in four patients. FEC uptake in the pelvic lymph nodes was found in the external iliac nodes in seven of 20 cases (35%), within the fossa obturatoria in four cases (20%), and in common iliac nodes in three patients (15%). Two cases with presacral nodes were detected.
The researchers found a survival rate of 94% at the median follow-up of 28 months. For primary tumors, relapse-free survival was 83% at 28 months, compared with 49% for recurrent tumors. Patients with primary tumors had a distant disease-free survival rate of 100% at 28 months, compared with 75% for patients with recurrent disease.
Two patients died during the follow-up period; for one patient, death occurred at 33.3 months due to bone metastases. The other patient died unexpectedly of unknown causes and without signs of prostate cancer at 17.5 months.
Based on the results, Wuerschmidt and colleagues concluded that FEC-PET/CT "could be helpful in dose escalation in prostate cancer, allowing boost doses greater than 60 Gy to metastatic lymph nodal regions if PET/CT-planned intensity-modulated and image-guided radiotherapy is used. Thus, there might be still a curative chance for selected patients with metastatic lymph nodes or recurrent disease."
The authors also noted that while molecular imaging with FEC-PET/CT is promising, careful interpretation of PET/CT findings and consideration of clinical data are necessary in decision-making, as the spatial resolution of current PET/CT scanners is still limited to tumors in the range of 5 to 8 mm.