Dutch researchers are reporting on a peptide receptor radiolabeled therapy (PRRT) that can decrease both tumor size and the severity of side effects in cancer patients in this month's issue of the Journal of Nuclear Medicine.
The study from Erasmus Medical Center in Rotterdam, the Netherlands, analyzed 265 patients with gastroenteropancreatic or bronchial neuroendocrine tumors. The tumors have an unpredictable biological behavior, so the time between their discovery to final diagnosis may be delayed, much to the detriment of patients (JNM, September 2011, Vol. 52:9, pp. 1361-1368).
Lead author Dr. Saima Khan and colleagues noted that for patients with gastroenteropancreatic or bronchial neuroendocrine tumors, median progression-free survival time after PRRT is 40 months.
All 265 patients in the study were treated with the radiolabeled pharmaceutical octreotate (lutetium-177 DOTA octreotate). Follow-up visits were scheduled at six weeks, three months, and six months after the last treatment cycle, and biannually thereafter.
The subjects completed a baseline questionnaire prior to therapy and continued to report their levels of fatigue, nausea and vomiting, pain, shortness of breath, insomnia, appetite loss, constipation, and diarrhea, as well as physical, emotional, cognitive, and social functioning during follow-up visits.
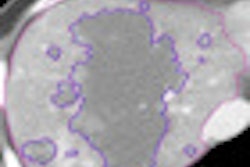
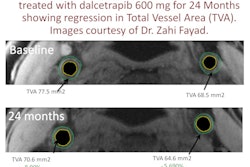
The researchers also used CT and MRI to categorize tumor response into three groups: a remission group, a stable disease group, and a progressive disease group.
Among all three groups, significant improvement was noted in emotional and social functioning, insomnia, appetite loss, and diarrhea. The most important improvements, in areas such as diarrhea, pain, and nausea and vomiting, were observed in patients who had tumor regression after therapy with octreotate, which suggests their benefits were a direct result of the treatment.
It would be "highly desirable" that future studies on the efficacy of antitumor agents, whether with radiopharmaceuticals or other drugs, also evaluate quality of life in the therapy's overall efficacy, Khan and colleagues recommended.