PET/CT with a carbon-11 (C-11) choline radiotracer is effective for evaluating prostate cancer, and in many cases it is better than conventional imaging for detecting the disease, according to three papers presented this week at the American Urological Association (AUA) annual meeting in Atlanta.
Dr. Jeffrey Karnes, senior author of all three papers, said in a statement that the three studies collectively represent "an important validation" of choline-PET/CT as an evaluation tool for patients with prostate cancer.
The three studies were retrospective reviews of prostate cancer patients at the Mayo Clinic who underwent choline-PET/CT imaging between September 2007 and November 2010.
In the first paper, Karnes and colleagues analyzed choline-PET/CT results along with findings from conventional imaging, targeted biopsies, or surgical resection. A total of 45 high-risk prostate cancer patients underwent choline-PET/CT for initial staging prior to treatment. In that setting, choline-PET/CT achieved a sensitivity, specificity, and positive predictive value of 100%, while negative predictive value was 93%.
Choline-PET/CT correctly predicted metastatic disease in 16 (89%) of 18 patients with confirmed metastasis. The modality produced two false-negative results in patients who were later found to have lymph node metastasis at radical prostatectomy. In addition, choline-PET/CT improved detection of metastasis over conventional imaging, such as x-ray, in five (11%) of 45 patients.
 |
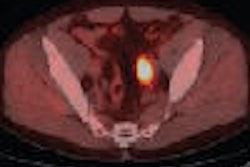
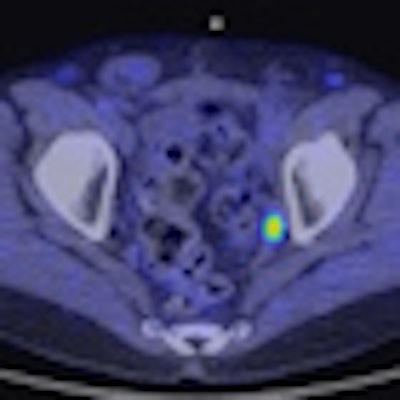
| Above is a traditional PET/CT scan of the pelvis of one individual. The image below is from a choline-PET/CT scan. The top image would appear negative to a radiologist, while the bottom scan is clearly positive for cancer, Karnes said. Images courtesy of Dr. Jeffrey Karnes. |
 |
In the second study, researchers evaluated 176 prostate cancer patients with disease recurrence following primary treatment failure. Among these patients, choline-PET/CT achieved a sensitivity of 93%, specificity of 76%, positive predictive value of 91%, and negative predictive value of 81%.
In all, 56 (32%) of 166 PET scans were determined to be clinically useful in detecting treatable lesions not identified by conventional imaging, resulting in an altered treatment plans for those patients.
Finally, in the third study, cancer recurrences were identified in 36 patients who underwent salvage surgery. Twenty-eight patients (77%) received metastasectomy for isolated disease recurrences and eight (23%) received salvage prostatectomy.
Choline-PET/CT reached a sensitivity of 88% and positive predictive value of 94%. In addition, PET was the only imaging modality to localize the site of recurrence in 14 (39%) of the 36 patients. However, PET failed to identify metastatic lesions among four patients (11%), all of whom were on androgen deprivation therapy at the time of the PET scan.
Negative surgical explorations were performed for two patients and choline-PET/CT did not accurately quantify the disease burden in four patients who had coexisting microscopic nodal metastases.
Based on the results, the researchers concluded that choline-PET/CT is accurate in detecting localized disease recurrences, which in certain cases are amenable to salvage surgical resection.