Mayo Clinic researchers have developed a modified protocol for low-dose molecular breast imaging (MBI) that cuts radiation dose by more than half. They have also developed an experimental technique that reduces dose to as little as 20% of what's currently used, according to two studies in the June issue of Medical Physics.
The researchers developed two techniques for improving the count sensitivity of commercially available MBI cameras. These involve redesigning the detector's collimation to optimize near-field imaging, and the use of a wide energy window to obtain images registered at lower energies with the systems' cadmium zinc telluride (CZT) digital detectors.
In one study using a phantom and in a second study with patients, lead author Dr. Carrie Hruska and colleagues achieved greater sensitivity, enhanced contrast-to-noise ratios, and the ability to detect small breast lesions with reduced doses of technetium-99m (Tc-99m) sestamibi.
Lower dose is needed
While MBI has shown promise as an adjunct to mammography for women with dense breasts, the modality's adoption depends in part on the reliable detection of lesions using low doses of Tc-99m sestamibi, with radiation levels comparable to mammography.
For the patient study, the researchers evaluated the redesign of the detector's collimation to optimize imaging in the near field and a wider energy window with very low doses of Tc-99m (Med Phys, June 2012, Vol. 39:6, pp. 3476-3483).
Following implementation of the count sensitivity improvement methods, Hruska and colleagues reduced the standard dose of Tc-99m for MBI at the Mayo Clinic from 740 MBq to 296 MBq. In some research cases, MBI was performed with 148 MBq of Tc-99m.
The researchers cited a previous study that found that injected Tc-99m sestamibi must be reduced to 148 MBq or less for radiation-induced cancer risk to be comparable to that of mammography. This injected dose is equivalent to an effective radiation dose of 1.2 mSv; the effective radiation dose for a two-view bilateral mammogram is 0.44 mSv for digital mammography and 0.56 mSv for film-screen mammography.
How did the lower dose affect system performance? Clinical image count density was compared between standard MBI with a 740-MBq Tc-99m dose, standard collimation, and a standard energy window to MBI with a 296-MBq Tc-99m dose, optimized collimation, and the wide energy window in 50 patients who were imaged using both protocols (LumaGem, Gamma Medica).
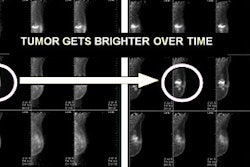
The researchers also evaluated lesion detection in a separate group of 32 patients who received MBI with a 296-MBq Tc-99m dose in dynamic mode, allowing the acquisition of images at 2.5-, 5.0-, 7.5-, and 10-minute intervals per breast view with proportionately reduced count densities.
The analysis found that low-dose MBI performed with 296-MBq Tc-99m with the enhanced collimation and wide energy window technology resulted in an average relative gain in count density of 4.2 ± 1.3, compared to standard MBI performed with 740 MBq.
In addition, low-dose MBI using 296-MBq Tc-99m achieved similar diagnostic accuracy at the acquisition times of 2.5, 5.0, 7.5, and 10 minutes per breast view with a median lesion size of 1.4 cm. The researchers also reported "near perfect" intrareader agreement between full 10-minute views and lower count density views.
The findings suggest that "further reductions in acquisition duration or administered dose may be achievable," Hruska and colleagues concluded.
Phantom study
In the phantom study, the researchers evaluated two dual-head CZT-based MBI systems -- LumaGem from Gamma Medica and Discovery NM 750b from GE Healthcare -- using the two count sensitivity improvement methods. Collimators, again, were optimized for dedicated breast imaging and a widened energy acceptance window was optimized for use with CZT (Med Phys, Vol. 39:6, pp. 3466-3475).
The study measured system sensitivity, spatial resolution, and tumor contrast-to-noise ratio, comparing standard collimation and energy window settings with optimal collimation and a wide energy window.
The researchers found that use of the optimized collimation and wide energy window increased system sensitivity to 3.6 counts/min/kBq for LumaGem and 2.8 counts/min/kBq for Discovery NM 750b.
However, there was a slight decline in spatial resolution with the new technique. LumaGem's spatial resolution was 4.8 mm with standard collimation and 5.6 mm with optimized collimation. Meanwhile, GE's Discovery NM 750b's spatial resolution went from 4.4 mm with standard collimation to 4.6 mm with the dose-optimized technique.
For both systems, at tumor depths of 1 cm and 3 cm, the optimized collimation and wide energy window "significantly improved" contrast-to-noise ratio compared to standard settings for tumors 8.0 mm and 9.2 mm in diameter, Hruska and colleagues noted.
"At the depth of 1 cm, optimized collimation and wide energy window also significantly improved [contrast-to-noise ratio] for 5.9-mm tumors on Discovery NM 750b," the authors added.
Based on the two studies, the group concluded that registered optimized collimation and a wide energy window "yield a substantial gain in count sensitivity and measurable gain in [contrast-to-noise ratio], with some loss in spatial resolution compared to the standard collimator designs and energy windows used on these two systems."
In addition, the count sensitivity improvements may allow MBI to be performed with a dose of 148-MBq Tc-99m, reducing unnecessary exposure to patients.
|
Study disclosures The Mayo Clinic Foundation and three authors obtain royalties from licensing arrangements between the Mayo Foundation and Gamma Medica. |