Cardiac FDG-PET/MRI is feasible on an integrated whole-body PET/MRI system, but the hybrid modality still must prove it adds clinical relevance to cases of ischemic heart disease, according to a study published online May 7 in Radiology.
The study from Essen University Hospital in Germany found good concordance with the simultaneous acquisition of FDG-PET and MR images regarding both cine and late gadolinium-enhanced imaging in patients with myocardial infarction.
However, despite the simultaneous MRI and PET acquisition, "consolidated cardiac PET/MRI protocols need to be established, as long examination times associated with fasting seem to compromise patient compliance" with the exams, wrote lead author Dr. Felix Nensa, from the department of diagnostic and interventional radiology and neuroradiology, and colleagues Radiology, May 7, 2013).
Cardiac feasibility study
The purpose of the study was to determine the feasibility of simultaneous acquisition of cardiac images on an integrated 3-tesla PET/MRI system, and to determine if the placement of the PET detector within the MRI's field of magnet strength would adversely affect clinical results.
The researchers evaluated 20 consecutive patients with ischemic heart disease who were referred for FDG-PET/MRI between May and December 2012. Among the 20 patients, 14 had confirmed acute ST-elevation myocardial infarction within four to 15 days after interventional revascularization, one had suspected non-ST-elevation myocardial infarction, and five had chronic myocardial infarction.
Ten of the 20 patients underwent additional cardiac PET/CT before their PET/MRI scan.
Individuals with contraindications for gadolinium-based contrast agents and general MRI conditions, such as claustrophobia, were excluded from the study. All patients were asked to detail any personal discomfort or side effects that occurred during the PET/MRI exam.
All imaging studies were performed with an integrated whole-body PET/MRI system with 3-tesla field strength (Biograph mMR, Siemens Healthcare) and the PET insert inside the MRI scanner. All MRI sequences were performed with phased-array body surface coils designed for the PET/MRI system.
For late gadolinium-enhanced qualitative imaging, patients received gadobutrol (Gadovist, Bayer HealthCare Pharmaceuticals) based on a dosage of 0.2 mmol/kg of body weight.
FDG-PET/MRI studies were performed after a fasting period of at least six hours, with FDG administered one hour before imaging with a mean of 202 (± 21) MBq. The scans began at a mean of 129 (± 41) minutes after FDG injection and included an electrocardiographically gated cardiac PET scan with one bed position and 3D image reconstruction.
For the FDG-PET/CT scans, an electrocardiographically gated cardiac PET/CT study was performed with a 128-slice CT unit (Biograph mCT, Siemens). PET scans began approximately 70 (± 12) minutes after FDG injection, with a mean of 211 (± 55) MBq.
Image comparisons
To compare the identification and characteristics of the infarcts between the two hybrid modalities, the researchers mapped the left ventricle with a 17-segment model, as recommended by the American Heart Association. Two-point scoring systems were used to assess myocardial tracer uptake, myocardial wall motion, and myocardial late enhancement in each segment.
In addition, the researchers measured the size of a patient's infarct zone by drawing regions on the late gadolinium-enhanced MR images and PET images, and it was expressed as a percentage of the entire left ventricular myocardium.
Nensa and colleagues were able to complete 19 of 20 cardiac PET/MRI scans. One patient with ST-elevation myocardial infarction did not finish due to claustrophobia. Total PET/MRI scan time without patient preparation and positioning was 53 (± 3) minutes, and all cardiac MR images were rated as diagnostic in quality.
The analysis of FDG-PET and MRI with the 17-segment model found "good concordance" of the left ventricle with both cine imaging and late gadolinium-enhanced imaging in 18 of the 19 patients.
Of the 306 segments evaluated, 97 (32%) were rated as infarcted on PET images, compared with 93 (30%) rated as infarcted on late gadolinium-enhanced images and 90 (29%) on cine images.
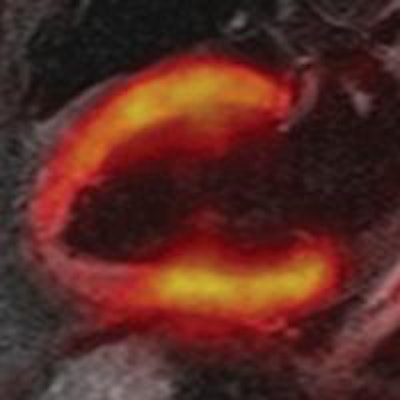
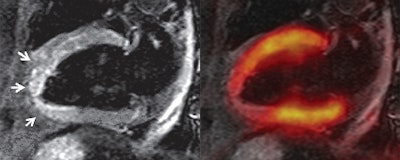
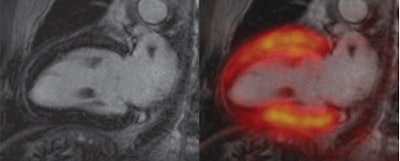 Two-chamber views show "stunned myocardium" in a 66-year-old patient with ST-elevation myocardial infarction and acute occlusion of the left anterior descending artery. Cardiac PET/MRI was performed seven days after intervention. Late gadolinium-enhanced image (top left) shows no infarction zone. Fused late gadolinium-enhanced and PET images (top right) show that tracer uptake was reduced in segments 13-15 and 17. T2-weighted MR image (bottom left) shows myocardial edema (arrows) that corresponded well with the area of reduced tracer uptake on the bottom right image. All images courtesy of Radiology.
Two-chamber views show "stunned myocardium" in a 66-year-old patient with ST-elevation myocardial infarction and acute occlusion of the left anterior descending artery. Cardiac PET/MRI was performed seven days after intervention. Late gadolinium-enhanced image (top left) shows no infarction zone. Fused late gadolinium-enhanced and PET images (top right) show that tracer uptake was reduced in segments 13-15 and 17. T2-weighted MR image (bottom left) shows myocardial edema (arrows) that corresponded well with the area of reduced tracer uptake on the bottom right image. All images courtesy of Radiology.
The size of the infarct zones averaged 22% of the entire left ventricular myocardium on PET images, compared with an average of 20% on late gadolinium-enhanced images.
Among the subgroup of 10 patients with an additional PET/CT scan, no significant difference in myocardial tracer uptake between PET/CT and PET/MR images was found.
In patient exit interviews, 16 patients cited long examination times (including patient preparation) as a source of discomfort. In addition, 11 patients cited the PET/MRI exam itself, i.e., noise, narrowness, and immobility, while 15 patients did not like having to fast.
Final conclusions
In summary, the PET/MRI device produced "high-quality cardiac MR imaging acquisitions," overcoming any technical issues of having the PET detector within the MRI's 3-tesla magnet field, Nensa and colleagues concluded.
"No negative side effects from the integrated imaging system design were observed," they noted.
The researchers were able to show "a close match" between FDG-PET and MRI in assessing myocardial viability and infarct quantification among patients with acute and chronic myocardial infarction.
"These findings demonstrate the feasibility of clinical cardiac MR imaging with an integrated PET/MRI device," they added. "However, to prove that the integrated design does not interfere with the performance of the device, a systematic intraindividual comparison with a comparable 3-tesla MRI system and identical sequence parameters is still needed."
Future studies should investigate whether hybrid FDG-PET/MRI of myocardial infarction can provide additional information compared with MRI or PET alone, according to the authors.