Using structural MRI and PET, researchers from New York University (NYU) may have found a link between sleep-disordered breathing and markers in cerebrospinal fluid that could indicate risk of Alzheimer's disease.
The findings add to the debate over whether Alzheimer's disease in its preclinical stages could lead to sleep-disordered breathing and explain the increased prevalence of sleep-disordered breathing in older people.
The study enrolled 68 cognitively normal elderly patients (mean age, 71.4), who underwent two nights of home monitoring for sleep-disordered breathing and were tested for at least one indicator of Alzheimer's disease.
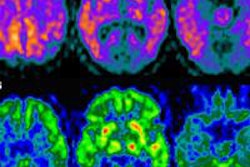
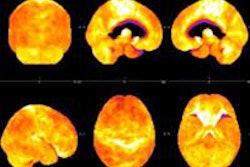
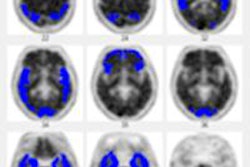
The researchers used FDG-PET to evaluate glucose metabolism, Pittsburgh Compound B (PiB) PET to measure amyloid load, and MRI to measure hippocampal volume.
The group only found a significant association between Alzheimer's and sleep-disordered breathing when they examined body weight, according to lead author Dr. Ricardo Osorio, a research assistant professor at NYU. Patients with a body mass index (BMI) less than 25 and sleep-disordered breathing had biomarkers of Alzheimer's risk, such as increased P-tau and T-tau in the cerebrospinal fluid, hippocampal atrophy, and glucose hypometabolism in Alzheimer's-vulnerable regions.
Among obese patients with BMI greater than 25, glucose hypometabolism at FDG-PET was also found in the medial temporal lobe, but it was not significant in other Alzheimer's-vulnerable regions.
Osorio and colleagues hope to conduct a two-year longitudinal study to test their hypothesis that very early-stage brain injury associated with these Alzheimer's biomarkers can lead to sleep-disordered breathing. The goal of the study would be to clarify any causality between sleep-disordered breathing and preclinical Alzheimer's disease in elderly patients.
The current study will be presented this week at the American Thoracic Society (ATS) conference in Philadelphia.